- Research
- Open access
- Published:
A framework of evidence-based decision-making in health system management: a best-fit framework synthesis
Archives of Public Health volume 80, Article number: 96 (2022)
Abstract
Background
Scientific evidence is the basis for improving public health; decision-making without sufficient attention to evidence may lead to unpleasant consequences. Despite efforts to create comprehensive guidelines and models for evidence-based decision-making (EBDM), there isn`t any to make the best decisions concerning scarce resources and unlimited needs. The present study aimed to develop a comprehensive applied framework for EBDM.
Methods
This was a Best-Fit Framework (BFF) synthesis conducted in 2020. A comprehensive systematic review was done via six main databases including PUBMED, Scopus, Web of Science, Science Direct, EMBASE, and ProQuest using related keywords. After the evidence quality appraisal, data were extracted and analyzed via thematic analysis. Results of the thematic analysis and the concepts generated by the research team were then synthesized to achieve the best-fit framework applying Carroll et al. (2013) approach.
Results
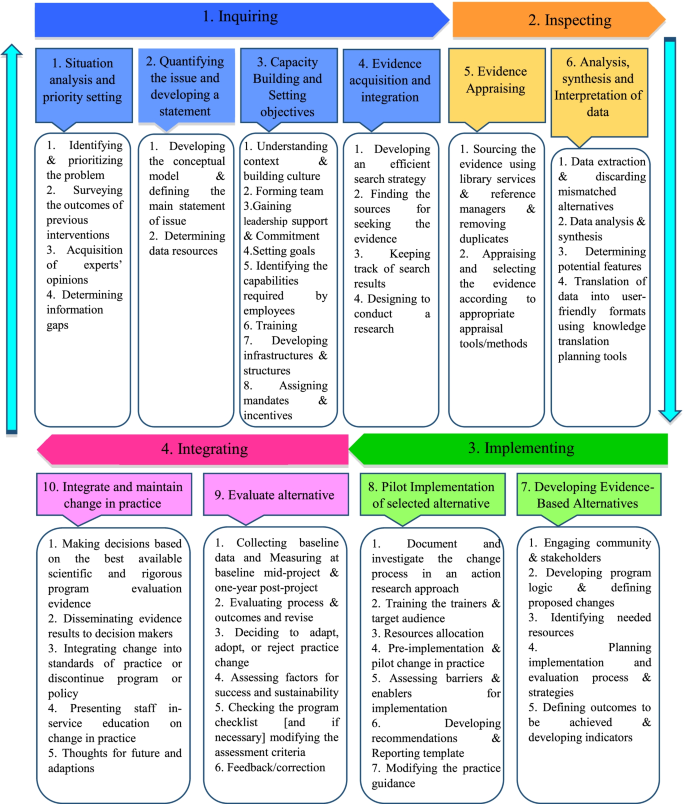
Four thousand six hundred thirteen studies were retrieved, and due to the full-text screening of the studies, 17 final articles were selected for extracting the components and steps of EBDM in Health System Management (HSM). After collecting, synthesizing, and categorizing key information, the framework of EBDM in HSM was developed in the form of four general scopes. These comprised inquiring, inspecting, implementing, and integrating, which included 10 main steps and 47 sub-steps.
Conclusions
The present framework provided a comprehensive guideline that can be well adapted for implementing EBDM in health systems and related organizations especially in underdeveloped and developing countries where there is usually a lag in updating and applying evidence in their decision-making process. In addition, this framework by providing a complete, well-detailed, and the sequential process can be tested in the organizational decision-making process by developed countries to improve their EBDM cycle.
Background
Globally, there is a growing interest in using the research evidence in public health policy-making [1, 2]. Public health systems are diverse and complex, and health policymakers face many challenges in developing and implementing policies and programs that are required to be efficient [1, 3]. The use of scientific evidence is considered to be an effective approach in the decision-making process [3,4,5]. Due to the lack of sufficient resources, evidence-based decision-making (EBDM) is regarded as a way to optimize costs and prevent wastes [6]. At the same time, the direct consequence of ignoring evidence is poorer health for the community [7].
Evidence suggests that health systems often fail to exploit research evidence properly, leading to inefficiencies, death or reduced quality of citizens’ lives, and a decline in productivity [8]. Decision-making in the health sector without sufficient attention to evidence may lead to a lack of effectiveness, efficiency, and fairness in health systems [9]. Instead, the advantages of EBDM include adopting cost-effective interventions, making optimal use of limited resources, increasing customer satisfaction, minimizing harm to individuals and society, achieving better health outcomes for individuals and society [10, 11], as well as increasing the effectiveness and efficiency of public health programs [12].
Using the evidence in health systems’ policymaking is a considerable challenging issue that many developed and developing countries are facing nowadays. This is particularly important in the latter, where their health systems are in a rapid transition [13]. For instance, although in 2012, a study in European Union countries showed that health policymakers rarely had necessary structures, processes, and tools to exploit research evidence in the policy cycle [14], the condition can be worse among the developing and the underdeveloped ones. For example, evidence-based policy-making in developing countries like those located in the Middle East can have more significant impacts [15, 16]. In such countries resources are generally scarce, so the policymakers' awareness of research evidence becomes more important [17]. In general, low and middle-income countries have fewer resources to deal with health issues and need quality evidence for efficient use of these resources [7].
Since the use of EBDM is fraught with the dilemma of most pressing needs and having the least capacity for implementation especially in developing countries [16], efforts have been made to create more comprehensive guidelines for EBDM in healthcare settings, in recent years [18]. Stakeholders are significantly interested in supporting evidence-based projects that can quickly prioritize funding allocated to health sectors to ensure the effective use of their financial resources [19,20,21]. However, it is unlikely that the implementation of EBDM in Health System Management (HSM) will follow the evidence-based medicine model [10, 22]. On the other hand, the capacity of organizations to facilitate evidence utilization is complex and not well understood [22], and the EBDM process is not usually institutionalized within the organizational processes [10]. A study in 2005 found that few organizations support the use of research evidence in health-related decisions, globally [23]. Weis et al. (2012) also reported there is insufficient information on EBDM in local health sectors [12]. In general, it can be emphasized that relatively few organizations hold themselves accountable for using research evidence in developing health policies [24]. To the best of our knowledge, there isn`t any comprehensive global and practical model developed for EBDM in health systems/organizations management. Accordingly, the present study aimed to develop a comprehensive framework for EBDM in health system management. It can shed the light on policymakers to access a detailed practical model and enable them to apply the model in actual conditions.
Methods
This was a Best Fit Framework (BFF) synthesis conducted in 2020 to develop a comprehensive framework for EBDM in HSM. Such a framework synthesis is achieved as a combination of the relevant framework, theory, or conceptual models and particularly is applied for developing a priori framework based on deductive reasoning [25]. The BFF approach is appropriate to create conceptual models to describe or express the decisions and behaviors of individuals and groups in a particular domain. This is distinct from other methods of evidence synthesis because it employs a systematic approach to create an initial framework for synthesis based on existing frameworks, models, or theories [25] for identifying and adapting theories systematically with the rapid synthesis of evidence [25, 26]. The initial framework can be derived from a relatively well-known model in the target field, or be formed by the integration of several existing models. The initial framework is then reduced to its key components that have shaped its concepts [25]. Indeed, the initial framework considers as the basis and it can be rebuilt, extended, or reduced based on its dimensions [26]. New concepts also emerge based on the researchers' interpretation of the evidence and ongoing comparisons of these concepts across studies [25]. This approach of synthesis possesses both positivist and interpretative perspectives; it provides the simultaneous use of the well-known strengths of both framework and evidence synthesis [27].
In order to achieve this aim the following methodological steps were conducted as follows:
Searching and selection of studies
In this step, we aimed to look for the relevant models and frameworks related to evidence-based decision-making in health systems management. The main research question was “what is the best framework for EBDM in health systems?” after defining the research question, the researchers searched for published studies on EBDM in HSM in different scientific databases with relevant keywords and constraints as inclusion and exclusion criteria from 01.01.2000 to 12.31.2020 (Table 1).
Inclusion and exclusion criteria
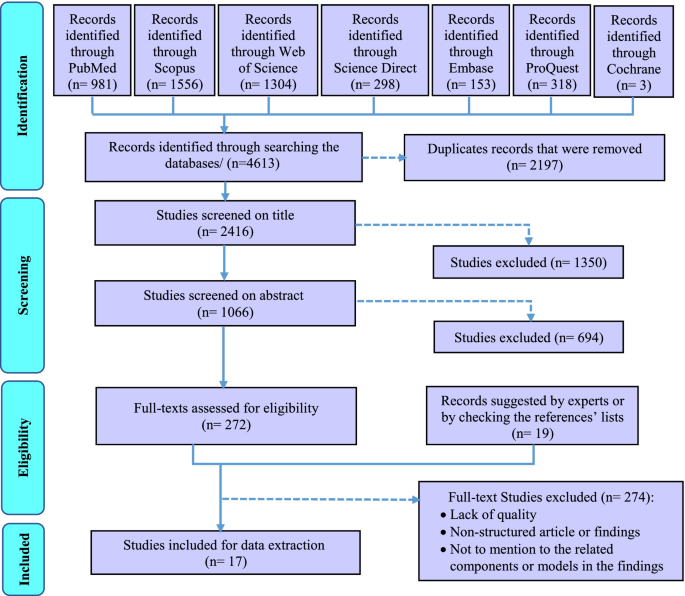
Inclusion criteria were determined as the studies that identify the components or develop a model or framework of EBDM in health organization in the form of original or review articles or dissertations, which were published in English and had a full text. The studies like book reviews, opinion articles, and commentaries that lacked a specific framework for conducting our review were excluded. During the search phase of the study, we attempted as much as possible to access studies that were not included in the search process or gray literature by reviewing the references lists of the retrieved studies or by contacting the authors of the articles or experts and querying them, as well as manually searching the related sites (Fig. 1).
Quality appraisal
The quality of the obtained studies was investigated using three tools for assessing the quality of various types of studies considering types and methods of the final include studies in systematic review. These tools were including Critical Appraisal Skills Program (CASP) for assessing the quality of qualitative researches [28], Scale for the Assessment of Narrative Review Articles (SANRA) [29], and The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers [30] (Table 3-Appendix).
Data extraction
After searching the studies from all databases and removing duplicates, the studies were independently reviewed and screened by two members (TS and MRAM) of the research team in three phases by the title, abstract, and then the full text of the articles. At each stage of the study, the final decision to enter the study to the next stage was based on agreement and, in case of disagreement, the opinion of the third person from the research team was asked (PB). Mendeley reference manager software was used to systematically search and screen relevant studies. The data from the included studies were extracted based on the study questions and accordingly, a form of the studies’ profile including the author's name, publication year, country, study title, type of study, and its conditions were prepared in Microsoft Excel software (Table 4-Appendix).
Synthesis and the conceptual model
In this step, a thematic analysis approach was applied to extract and analyze the data. For this purpose, first, the texts of the selected studies were read several times, and the initial qualitative codes or thematic concepts, according to the determined keywords and based on the research question, were found and labeled. Then these initial thematic codes were reviewed to achieve the final codes and they were integrated and categorized to achieve the final main themes and sub-themes, eventually. The main and the sub-themes are representative of the main and sub-steps of EBDM. At the last stage of the synthesis, the thematic analysis was finalized with 8 main themes and all the main and the sub-themes were tabulated (Table 5-Appendix).
Creation of a new conceptual framework
For BFF synthesis in the present study, we compared the existing models and tried to find a model that fits the best. Three related models that appeared to be relatively well-suited to the purpose of this study to provide a complete, comprehensive, and practical EBDM model in HSM were found. According to the BFF instruction in Carroll et al. (2013) study [25], we decided to use all three models as the basis for the best fit because any of those models were not complete enough and we could give no one an advantage over others. Consequently, the initial model or the BFF basis was formed and the related thematic codes were classified according to the category of this basis as the main themes/steps of EBDM in HSM (Table 5-Appendix). Then, the additional founded thematic codes were added and incorporated to this basis as the other main steps and the sub-steps of the EBDM in HSM according to the research team and some details in the form of sub-steps were added by the research team to complete the synthesized framework. Eventually, a comprehensive practical framework consisting of 10 main steps and 47 sub-steps was created with the potentiality of applying and implementing EDBM in HSM that we categorized them into four main phases (Table 6-Appendix).
Testing the synthesis: comparison with the a priori models, dissonance and sensitivity
In order to assess the differences between the priori framework and the new conceptual framework, the authors tried to ask some experts’ opinions about the validity of the synthesized results. The group of experts has included eight specialists in the field of health system management or health policy-making. These experts have been chosen considering their previous research or experience in evidence-based decision/policy making performance/management (Table 2). This panel lasted in two three-hour sessions. The finalized themes and sub-themes (Table 6-Appendix) and the new generated framework (Fig. 3) were provided to them before each session so that they could think and then in each meeting they discussed them. Finally, all the synthesized themes and sub-themes resulted were reviewed and confirmed by the experts.
Ethical considerations
To prevent bias, two individuals carried out all stages of the study such as screening, data extraction, and data analysis. The overall research project related to this manuscript was approved by the medical ethics conceal of the research deputy of Shiraz University of Medical Sciences with approval number IR.SUMS.REC.1396–01-07–14184, too.
Results
The initial search across six electronic databases and the Cochrane library yielded 4613 studies. After removing duplicates, 2416 studies were assessed based on their titles. According to the abstract screening of the 1066 studies that remained after removing the irrelevant titles, 291 studies were selected and were entered into the full-text screening phase. Due to full-text screening of the studies, 17 final studies were selected for extracting the components and steps of EBDM in HSM (Fig. 1). The features of these studies were summarized in Table 4-Appendix (see supplementary data). Furthermore, according to the quality appraisal of the included studies, the majority of them had an acceptable level of quality. These results have been shown in Table 3-Appendix.
Results of the thematic analysis of the evidence (Table 5-Appendix) along with the concepts proposed and added by the research team according to the focus-group discussion of the experts were shown in Table 6-Appendix. Accordingly, the main steps and related sub-steps of the EBDM process in HSM were defined and categorized.
After collecting, synthesizing, and categorizing thematic concepts, incorporating them with the initial models, and adding the additional main steps and sub-steps to the basic models, the final synthesized framework as a best-fit framework for EBDM in HSM was developed in the form of four general phases of inquiring, inspecting, implementing, and integrating and 10 main steps (Fig. 2). For better illustration, this framework with all the main steps and 47 sub-steps has been shown in Fig. 3, completely.
Discussion
In the present study, a comprehensive framework for EBDM in HSM was developed. This model has different distinguishing characteristics than the formers. First of all, this is a comprehensive practical model that combined the strengths and the crucial components of the limited number of previous models; second, the model includes more details and complementary steps and sub-steps for full implementation of EBDM in health organizations and finally, the model is benefitted from a cyclic nature that has a priority than the linear models. Concerning the differences between the present framework and other previous models in this field, it must be said that most of the previous models related to EBDM were presented in the scope of medicine (that they were excluded from our SR according to the study objectives and exclusion criteria). A significant number of those models were proposed for the scope of public health and evidence-based practice, and only a limited number of them focused exactly on the scope of management and policy/decision making in health system organizations.
Given that the designed model is a comprehensive 10-step model, it can be used in some way at all levels of the health system and even in different countries. However, there will be a difference here, given that this framework provides a practical guide and a comprehensive guideline for applying evidence-based decision-making approach in health systems organizations, at each level of the health system in each country, this management approach can be applied depending on their existing infrastructure and the processes that are already underway (such as capacity building, planning, data collection, etc.), and at the same time, with a general guide, they can provide other infrastructure as well as the prerequisites and processes needed to make this approach much more possible and applicable.
It is true that evidence-based management is different from evidence-based medicine and even more challenging (due to lack of relevant data, greater sensitivity in data collection and their accuracy, lack of consistency and lack of transparency in the implementation of evidence-based decision-making in management rather than evidence-based medicine, etc.). Still, the general framework provided in this article can be used to help organizations that really want to act and move forward through this approach.
Furthermore, based on the findings, most of the previous studies only referred to some parts of the components and steps of the EBDM in health organizations and neglected the other parts or they were not sufficiently comprehensive [31,32,33,34,35,36,37,38,39,40]. Most of the previous models did not mention the necessary sub-steps, tools, and practical details for accurate and complete implementation of the EBDM, which causes the organizations that want to use these models, will be confused and cannot fully implement and complete the EBDM cycle. Among the studies that have provided a partly complete model than the other studies, were the studies by Brownson (2009), Yost (2014), and Janati (2018) [3, 41, 42]. Consequently, the combination of these three studies has been used as the initial framework for the best-fit synthesis in the present study.
Likewise, the models presented by Brownson (2009) and Janati (2018) were only limited to the six or seven key steps of the EBDM process, and they did not mention the details required for doing in each step, too [3, 4, 42]. Also, the model presented in the study of Janati (2018) was linear, and the relationships between the EBDM components were not well considered [42, 43]; however, the model presented in this study was recursive. Also, in Yost's study (2014), despite the 7 main steps of EBDM and some details of each of the steps, the proposed process was not schematically drawn in the form of a framework and therefore the relationships between steps and sub-steps were not clear [41]. According to what was discussed, the best-fit framework makes the possibility of concentrating the fragmented models to a comprehensive one that can be fully applied and evaluated by the health systems policymakers and managers.
In the present study, the framework of EBDM in HSM was developed in the form of four general scopes of inquiring, inspecting, implementing, and integrating including 10 main steps and 47 sub-steps. These scopes were discussed as follows:
Inquiring
In the first step, “situation analysis and priority setting”, the most frequently cited sub-step was identifying and prioritizing the problem. Accordingly, Falzer (2009), emphasized the importance of identifying the decision-making conditions and the relevant institutions and determining their dependencies as the first steps of EBDM [44]. Aas (2012) has also cited the assessment of individuals and problem status and problem-finding as the first steps of EBDM [34]. Moreover, the necessity of identifying the existing situation and issues and prioritizing them has been emphasized as the initial steps in most management models such as environmental analysis in strategic planning [45].
Despite considering the opinions and experience of experts and managers as one of the important sources of evidence for decision-making [42, 46,47,48,49,50], many studies did not mention this sub-step in the EBDM framework. Hence, the present authors added the acquisition of experts’ opinions as a sub-step of the first step because of its important role in achieving a comprehensive view of the overall situation.
In the second step, “quantifying the issue and developing a statement”, “Developing the conceptual model for the issue” was more addressed [37, 41, 47]. In addition, the authors to complete this step added the fourth sub-step, “Defining the main statement of issue”. This is because that most of the problems in health settings may have a similar value for managers and decision-makers and quantifying them can be used as a criterion for more attention or selecting the problem as the main issue to solve.
The third step, “Capacity building and setting objectives”, was not seen in many other included studies as a main step in EBDM, however, the present authors include this as a main step because without considering the appropriate objectives and preparing necessary capacities and infrastructures, entering to the next steps may become problematic. Moreover, in numerous studies, factors such as knowledge and skills of human resources, training, and the availability of the essential structures and infrastructures have been identified as facilitators of EBDM [51,52,53,54,55]. According to this justification, they are included in the present framework as sub-steps of the third step.
Considering the third step and based on the knowledge extracted from the previous studies, the three sub-steps of “understanding context and Building Culture” [56, 57], “gaining the support and commitment of leaders” [39, 57, 58], and “identifying the capabilities required by employees and their skills weaknesses” [58,59,60] were the most important sub-steps in this step of EBDM framework. In this regard, Dobrow (2004) has also stated that the two essential components of any EBDM are the evidence and context of its use [32]. Furthermore, Isfeedvajani (2018) stated that to overcome barriers and persuade hospital managers and committees to apply evidence-based management and decision-making, first and foremost, creating and promoting a culture of "learning through research" was important [61].
The present findings showed that in the fourth main step, “evidence acquisition and integration”, the most important sub-step was “finding the sources for seeking the evidence” [39,40,41, 60, 62, 63]. Concerning the sources for the use of evidence in decision-making in HSM, studies have cited numerous sources, most notably scientific and specialized evidence such as research, articles, academic reports, published texts, books, and clinical guidelines [39, 64, 65]. After scientific evidence, using the opinions and experiences of experts, colleagues, and managers [42, 46, 49, 66] as well as the use of census and local level data [49, 66, 67], and other sources such as financial [67], political [42, 49] and evaluations [49, 68] data were cited.
Inspecting
The fifth step of the present framework, “evidence appraising”, was emphasized by previous literature; for instance, Pierson (2012) pointed to the use of library services in EBDM [69]. Appraising and selecting the evidence according to appropriate appraisal tools/methods was cited the most. International and local evidence is confirmed that ignoring these criteria can lead to serious faults in the process of decision and policy-making [70, 71].
Furthermore, the sixth step, “analysis, synthesis, and interpretation of data”, was mentioned in many included studies [36, 39, 41, 42, 57, 59, 72]. This step emphasized the role of analysis and synthesis of data in the process of generation applied and useful information. It is obvious that the local interpretation according to different contexts may lead to achieving such kind of knowledge that can be used as a basis for local EBDM in HSM.
Implementing
The third scope consisted of the seventh and eighth steps of the EBDM process in HSM. In the seventh step, “developing evidence-based alternatives”, the issue of involving stakeholders in decision-making and subsequently, planning to design and implementation of the process and evaluation strategies had been focused by the previous studies [58, 60, 62, 63, 73]. Studies by Belay (2009) and Armstrong (2014) had also emphasized the need to use stakeholder and public opinion as well as local and demographic data in decision-making [49, 67].
“Pilot-implementation of selected alternatives” was the eighth step of the framework. Some key sub-steps of this step were resources allocation [58], Pre-implementation and pilot change in practice and assessing barriers and enablers for implementation [40] that indicated the significance of testing the strategies in a pilot stage as a pre- requisition of implementing the whole alternatives. It is obvious that without attention to the pilot stage, adverse and unpleasant outcomes may occur that their correction process imposes many financial, organizational, and human costs on the originations. In addition, a study explained that one of the strategies of the decision-makers to measure the feasibility of the policy options was piloting them, which had a higher chance of being approved by the policymakers. Also, pilot implementation in smaller scales has been recommended in public health in cases of lack of sufficient evidence [74].
Integrating
This last scope consists of the ninth and tenth steps. The main sub-step of the ninth step, “evaluating alternatives”, was to evaluating process and outcomes and revise. After a successful implementation of the pilot, this step can be assured that the probable outcomes may be achieved and this evaluation will help the decision and policymakers to control the outcomes, effectively. Also, it impacts the whole target program and proposes some correcting plans through an accurate feedback process, too. Pagoto (2007) explained that a facilitator for EBDM would be an efficient and user-friendly system to assess utilization, outcomes, and perceived benefits [55].
Also, the tenth step, “integrating and maintaining change in practice”, was not considered as a major step in previous models, too, while it is important to maintain and sustain positive changes in organizational performance. In this regard, Ward (2011) also suggested several steps to maintain and sustain the widespread changes in the organization, including increasing the urgency and speed of action, forming a team, getting the right vision, negotiating for buy-in, empowerment, short-term success, not giving up and help to make a change stick [35]. Finally, the most important sub-steps that could be mentioned in this step were the dissemination of evidence results to decision-makers and the integration of changes made to existing standards and performance guidelines. Liang (2012) had also emphasized the importance of translating existing evidence into useful practices as well as disseminating them [47]. In addition, the final sub-step, “feedback and feedforward towards the EBDM framework”, was explained by the authors to complete the framework.
Some previous findings showed that about half and two-thirds of organizations do not regularly collect related data about the use of evidence, and they do not systematically evaluate the usefulness or impact of evidence use on interventions and decisions [75]. The results of a study conducted on healthcare managers at the various levels of an Iranian largest medical university showed that the status of EBDM is not appropriate. This problem was more evident among physicians who have been appointed as managers and who have less managerial and systemic attitudes [76]. Such studies, by concerning the shortcomings of current models for EBDM in HSM or even lack of a suitable and usable one, have confirmed the necessity of developing a comprehensive framework or model as a practical guide in this field. Consequently, existing and presenting such a framework can help to institutionalize the concept of EBDM in health organizations.
In contrast, results of Lavis study (2008) on organizations that supported the use of research evidence in decision-making reported that more than half of the organizations (especially institutions of health technology assessment agencies) may use the evidence in their process of decision-making [75], so applying the present framework for these organizations can be recommended, too.
Limitations
One of the limitations of the present study was the lack of access to some studies (especially gray literature) related to the subject in question that we tried to access them by manual searching and asking from some articles’ authors and experts. In addition, most of the existing studies on EBDM were limited to examining and presenting results on influencing, facilitating, or hindering factors or they only mentioned a few components in this area. Consequently, we tried to search for studies from various databases and carefully review and screen them to make sure that we did not lose any relevant data and thematic code. Also, instead of one model, we used four existing models as a basis in the BFF synthesis so that we can finally, by adding additional codes and themes obtained from other studies as well as expert opinions, provide a comprehensive model taking into account all the required steps and details. Also, the framework developed in this study is a complete conceptual model made by BFF synthesis; however, it may need some localization, according to the status and structure of each health system, for applying it.
Conclusions
The present framework provides a comprehensive guideline that can be well adapted for implementing EBDM in health systems and organizations especially in underdeveloped and developing countries where there is usually a lag in updating and applying evidence in their decision-making process. In addition, this framework by providing a complete, well-detailed, sequential and practical process including 10 steps and 56 sub-steps that did not exist in the incomplete related models, can be tested in the organizational decision-making process or managerial tasks by developed countries to improve their EBDM cycle, too.
Availability of data and materials
All data in a form of data extraction tables are available from the corresponding author on a reasonable request.
Abbreviations
- EBDM:
-
Evidence-based decision-making
- HSM:
-
Health System Management
- BFF:
-
Best-Fit Framework
References
Rychetnik L, Bauman A, Laws R, King L, Rissel C, Nutbeam D, et al. Translating research for evidence-based public health: Key concepts and future directions. J Epidemiol Community Health. 2012;66(12):1187–92.
Nutbeam D, Boxall AM. What influences the transfer of research into health policy and practice? Observations from England and Australia. Public Health. 2008;122(8):747–53.
Brownson RC, Fielding JE, Maylahn CM. Evidence-Based Public Health: A Fundamental Concept for Public Health Practice. Annu Rev Public Health [Internet]. 2009;30(1):175–201. https://doi.org/10.1146/annurev.publhealth.031308.100134.
Brownson RC, Gurney JG, Land GH. Evidence-based decision making in public health. J Public Heal Manag Pract [Internet]. 1999 [cited 2018 May 26];5(5):86–97. Available from: https://books.google.com/books?hl=en&lr=&id=yxRgAwAAQBAJ&oi=fnd&pg=PA133&dq=+criteria+OR+health+%22evidence+based+decision+making%22&ots=hiqVNQtF24&sig=jms9GsBfw6gz1cN2FQXzCBZvmMQ
McGinnis JM. ‘Does Proof Matter? Why Strong Evidence Sometimes Yields Weak Action.’ Am J Heal Promot. 2001;15(5):391–396. Available from: https://doi.org/10.4278/0890-1171-15.5.391.
Majdzadeh R, Yazdizadeh B, Nedjat S, Gholami J, Ahghari S, R. M, et al. Strengthening evidence-based decision-making: Is it possible without improving health system stewardship? Health Policy Plan [Internet]. 2012 Sep 1 [cited 2018 May 15];27(6):499–504. Available from: https://doi.org/10.1093/heapol/czr072
WHO EIPNET. Using evidence and innovation to strengthen policy and practice. 2008.
Ellen ME, Léon G, Bouchard G, Lavis JN, Ouimet M, Grimshaw JM. What supports do health system organizations have in place to facilitate evidence-informed decision-making? A qualitative study. Implement Sci. 2013;8(1):84.
Oxman AD, Lavis JN, Lewin S, Fretheim A. What is evidence-informed policymaking? Health Res Policy Sys. 2009;7:1–7.
Armstrong R, Waters E, Dobbins M, Anderson L, Moore L, Petticrew M, et al. Knowledge translation strategies to improve the use of evidence in public health decision making in local government: Intervention design and implementation plan. Implement Sci [Internet]. 2013;8(1):1. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84885076767&doi=10.1186%2F1748-5908-8-121&partnerID=40&md5=dddaf4029205c63877a3e6ecf28f7762
Waters E, Armstrong R, Swinburn B, Moore L, Dobbins M, Anderson L, et al. An exploratory cluster randomised controlled trial of knowledge translation strategies to support evidence-informed decision-making in local governments (The KT4LG study). BMC Public Health [Internet]. 2011;11(1):34. Available from: http://www.biomedcentral.com/1471-2458/11/34
Imani-Nasab MH, Yazdizadeh B, Salehi M, Seyedin H, Majdzadeh R. Validity and reliability of the Evidence Utilisation in Policymaking Measurement Tool (EUPMT). Heal Res Policy Syst. 2017;15(1):1–11.
El-Jardali F, Lavis JN, Ataya N, Jamal D, Ammar W, Raouf S. Use of health systems evidence by policymakers in eastern mediterranean countries: Views, practices, and contextual influences. BMC Health Serv Res. 2012;12(1):200.
Ettelt S, Mays N. Health services research in Europe and its use for informing policy. J Health Serv Res Policy [Internet]. 2011 Jul 29 [cited 2019 Jun 29];16(2_suppl):48–60. Available from: https://doi.org/10.1258/jhsrp.2011.011004
Sutcliffe S. Evidence-Based Policymaking: What is it? How does it work? What relevance for developing countries? 2005.
Campbell DM, Redman S, Jorm L, Cooke M, Zwi AB, Rychetnik L. Increasing the use of evidence in health policy: Practice and views of policy makers and researchers. Aust New Zealand Health Policy. 2009;6(1):1–11.
WHO. Supporting the Use of Research Evidence (SURE) for Policy in African Health Systems. 2007:1–72.
Health Public Accreditation Board. Public Health Accreditation Board STANDARDS : AN OVERVIEW. 2012.
Riley WJ, Bender K, Lownik E. Public health department accreditation implementation: Transforming public health department performance. Am J Public Health. 2012;102(2):237–42.
Liebman JB. Building on Recent Advances in Evidence-Based Policymaking. 2013:36. Available from: http://www.americaachieves.org/9F42769C-3A65-4CCB-8466-E7BFD835CFE7/FinalDownload/DownloadId-0AB31816953C7B8AFBD2D15DFD39D5A8/9F42769C-3A65-4CCB-8466-E7BFD835CFE7/docs/RFA/THP_Liebman.pdf
Jacobs J a, Jones E, Gabella B a, Spring B, Brownson C. Tools for Implementing an Evidence-Based Approach in Public Health Practice. Prev Chronic Dis [Internet]. 2012;9(1):1–9. Available from: https://doi.org/10.5888/pcd9.110324
Kothari A, Edwards N, Hamel N, Judd M. Is research working for you? validating a tool to examine the capacity of health organizations to use research. Implement Sci. 2009;4(1):1–9.
Oxman AD, Bjørndal A, Becerra-Posada F, Gibson M, Block MAG, Haines A, et al. A framework for mandatory impact evaluation to ensure well informed public policy decisions. Lancet. 2010;375(9712):427–31. Available from: https://doi.org/10.1016/S0140-6736(09)61251-4
Oxman AD, Vandvik PO, Lavis JN, Fretheim A, Lewin S. SUPPORT Tools for evidence-informed health Policymaking (STP) 2: Improving how your organisation support the use of research evidence to inform policymaking. Chinese J Evidence-Based Med. 2010;10(3):247–54.
Carroll C, Booth A, Leaviss J, Rick J. “ Best fit ” framework synthesis : refining the method. BMC Med Res Methodol. 2013;13(1):1 Available from: BMC Medical Research Methodology.
Carroll C, Booth A, Cooper K. A worked example of “ best fit ” framework synthesis : A systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol. 2011;11:29.
Barnett-page E, Thomas J. Methods for the synthesis of qualitative research : a critical review. BMC Med Res Methodol 9. 2009;59:1–26.
Public Health Resource Unit. Critical Appraisal Skills Programme (CASP) making sense of evidence;10 questions to help you make sense of qualitative research. Public Health. 2006.
Baethge C, Goldbeck-Wood S, Mertens S. SANRA—a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019;4(1):2–8.
Hong Q, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT), Version 2018. User guide. McGill [Internet]. 2018;1–11. Available from: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf%0Ahttp://mixedmethodsappraisaltoolpublic.pbworks.com/
Titler MG. The Iowa Model of evidence-based practice to promote quality care. 2001.
Dobrow MJ, Goel V, Upshur REG. Evidence-based health policy: context and utilisation. Soc Sci Med [Internet]. 2004;58(1):207–17. Available from: http://www.sciencedirect.com/science/article/pii/S0277953603001667
Kohatsu ND, Robinson JG, Torner JC. Evidence-based public health: An evolving concept. Am J Prev Med. 2004;27(5):417–21.
Aas RW, Alexanderson K. Challenging Evidence-based Decision-making: A Hypothetical Case Study about Return to Work. Occup Ther Int. 2012 [cited 2018 May 28];19(1):28–44. Available from: https://doi.org/10.1002/oti.326
Ward M. Evidence-informed decision making in a public health setting. Healthc Manag Forum. 2011;24(1 SUPPL):S8.
Champagne F, Lemieux-Charles L, Duranceau M-F, MacKean G, Reay T. Organizational impact of evidence-informed decision making training initiatives: A case study comparison of two approaches. Implement Sci [Internet]. 2014;9(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84900004312&doi=10.1186%2F1748-5908-9-53&partnerID=40&md5=df5573f17e19ef002d67cf669059aef4
Wright AL, Zammuto RF, Liesch PW, Middleton S, Hibbert P, Burke J, et al. Evidence-based Management in Practice: Opening up the Decision Process, Decision-maker and Context. Br J Manag. 2016;27(1):161–78. Available from: https://doi.org/10.1111/1467-8551.12123
Stamatakis KA, Ferreira Hino AA, Allen P, McQueen A, Jacob RR, Baker EA, et al. Results from a psychometric assessment of a new tool for measuring evidence-based decision making in public health organizations. Eval Program Plann [Internet]. 2017 Feb [cited 2018 May 16];60:17–23. Available from: http://linkinghub.elsevier.com/retrieve/pii/S014971891630009X
Harris C, Allen K, Waller C, Dyer T, Brooke V, Garrubba M, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 7: supporting staff in evidence-based decision-making, implementation and evaluation in a local healthcare setting. BMC Health Serv Res [Internet]. 2017 Dec 21 [cited 2018 May 19];17(1):430. Available from: https://doi.org/10.1186/s12913-017-2388-8
Harris C, Garrubba M, Melder A, Voutier C, Waller C, King R, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 8: Developing, implementing and evaluating an evidence dissemination service in a local healthcare setting. BMC Health Serv Res [Internet]. 2018;18(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85042873576&doi=10.1186%2Fs12913-018-2932-1&partnerID=40&md5=2daa5bbd3ccddf299f7b9d527b6105af
Yost J, Dobbins M, Traynor R, DeCorby K, Workentine S, Greco L. Tools to support evidence-informed public health decision making. BMC Public Health [Internet]. 2014 Dec 18 [cited 2018 May 28];14(1):728. Available from: https://bmcpublichealth.biomedcentral.com/articles/https://doi.org/10.1186/1471-2458-14-728
Janati A, Hasanpoor E, Hajebrahimi S, Sadeghi- H, Khezri A. An Evidence-Based Framework for Evidence-Based Management in Healthcare Organizations : A Delphi Study. Ethiop J Heal Sci. 2018;28(3):305–14.
Rosswurm MA, Larrabee JH. A Model for Change to Evidence-Based Practice. J Nurs Scholarsh. 1999;31(4):317–22.
Falzer PR, Garman MD. A conditional model of evidence-based decision making. J Eval Clin Pract [Internet]. 2009 Dec [cited 2018 May 19];15(6):1142–51. Available from: http://doi.wiley.com/https://doi.org/10.1111/j.1365-2753.2009.01315.x
Ginter PM, Duncan WJ, Swayne LE. Strategic management of health care organizations. 8th Edition. Hoboken: John Wiley & Sons, Inc. 2018. p. 40.
Humphries S, Stafinski T, Mumtaz Z, Menon D. Barriers and facilitators to evidence-use in program management: a systematic review of the literature. BMC Health Serv Res [Internet]. 2014 Dec 14 [cited 2018 May 16];14(1):171. Available from: http://bmchealthservres.biomedcentral.com/articles/https://doi.org/10.1186/1472-6963-14-171
Liang Z, Howard PF, Leggat SG, Murphy G. A framework to improve evidence-informed decision-making in health service management. Aust Heal Rev [Internet]. 2012;36(3):284–9. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84865450745&doi=10.1071%2FAH11051&partnerID=40&md5=c42d56774cd486b8df8a5e4afec33a6a
Kohn MK, Berta W, Langley A, Davis D. Evidence-based decision making in health care settings: From theory to practice [Internet]. Vol. 11, Advances in Health Care Management. Emerald Group Publishing Ltd; 215–234 p. Available from: 2011. https://doi.org/10.1108/S1474-8231(2011)0000011012.
Armstrong R, Waters E, Moore L, Dobbins M, Pettman T, Burns C, et al. Understanding evidence: a statewide survey to explore evidence-informed public health decision-making in a local government setting. Implement Sci [Internet]. 2014;9(1):188. Available from: http://implementationscience.biomedcentral.com/articles/https://doi.org/10.1186/s13012-014-0188-7
McDiarmid M, Sandra K, Binns M. Evidence-based administrative decision making and the Ontario hospital CEO: information needs, seeking behaviour, and access to sources. JCHLA / JABSC [Internet]. 2007 [cited 2018 May 28];28:63–72. Available from: https://ejournals.library.ualberta.ca/index.php/jchla/article/viewFile/24060/17884
Brownson RC, Allen P, Duggan K, Stamatakis KA, Erwin PC. Fostering more-effective public health by identifying administrative evidence-based practices: A review of the literature. Am J Prev Med [Internet]. 2012;43(3):309–19. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84865688888&doi=10.1016%2Fj.amepre.2012.06.006&partnerID=40&md5=a843f04e58b619ab9355a98bbfeef51a
Moussata CO. Evidence-Based Management and its Influence on the Practices of Senior Leaders of Hospitals in the Denver Metropolitan Area [Internet]. ProQuest Dissertations and Theses. [Ann Arbor]: Colorado Technical University; 2017 [cited 2018 May 19]. Available from: https://search.proquest.com/docview/1967189422?accountid=41313
Ward M, Mowat D. Creating an organizational culture for evidence-informed decision making. Healthc Manag Forum [Internet]. 2012;25(3):146–50. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84867778644&doi=10.1016%2Fj.hcmf.2012.07.005&partnerID=40&md5=42f06b7236a4a1cd6a4739c7e1900764
Sosnowy CD, Weiss LJ, Maylahn CM, Pirani SJ, Katagiri NJ. Factors affecting evidence-based decision making in local health departments. Am J Prev Med [Internet]. 2013 Dec [cited 2018 May 19];45(6):763–8. Available from: http://dx.doi.org/https://doi.org/10.1016/j.amepre.2013.08.004
Pagoto SL, Spring B, Coups EJ, Mulvaney S. Barriers and Facilitators of Evidence-Based Practice Perceived by Behavioral Science Health Professionals. 2007;63(7):695–705.
Weiss L, Sosnowy C, Maylahn C, Katagiri N, Pirani S. Evidence-Based Decision Making in Local Health Departments Evidence-Based Decision Making in Local Health Departments. Front Public Heal Serv Syst Res. 2012;1(3):1–7.
Liang Z, Howard PF, Leggat SG, Murphy G. A framework to improve evidence-informed decision-making in health service management. Aust Heal Rev [Internet]. 2012;36(3):284–9. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84865450745&doi=10.1071%2FAH11051&partnerID=40&md5=c42d56774cd486b8df8a5e4afec33a6a
Lester L, Haby MM, Chapman E, Kuchenmüller T. Evaluation of the performance and achievements of the WHO Evidence-informed Policy Network (EVIPNet) Europe. Heal Res policy Syst. 2020;18(1):109.
Aas RW, Alexanderson K. Challenging evidence-based decision-making: A hypothetical case study about return to work. Occup Ther Int [Internet]. 2012 Mar [cited 2018 May 28];19(1):28–44. Available from: https://doi.org/10.1002/oti.326
Daouk-Öyry L, Sahakian T, van de Vijver F. Evidence-Based Management Competency Model for Managers in Hospital Settings. Br J Manag. 2020;00:1–20.
Isfeedvajani MS. Evidence-Based Management and its Application in the Hospital Management Process. Hosp Pract Res [Internet]. 2018 [cited 2018 May 28];3(2):35–6. Available from: http://jhpr.ir/article_60533_8313dd6afa580ef2afa689e6984c8844.pdf
Armstrong R, Waters E, Moore L, Dobbins M, Pettman T, Burns C, et al. Understanding evidence: a statewide survey to explore evidence-informed public health decision-making in a local government setting. Implement Sci [Internet]. 2014 Dec 14 [cited 2018 May 28];9(1):188. Available from: https://doi.org/10.1186/s13012-014-0188-7
Uneke CJ, Sombie I, Johnson E, Uneke BI, Okolo S. Promoting the use of evidence in health policymaking in the ECOWAS region: the development and contextualization of an evidence-based policymaking guidance. Global Health [Internet]. 2020;16(1):73. Available from: http://www.embase.com/search/results?subaction=viewrecord&id=L632558076&from=export
Janati A, Hasanpoor E, Hajebrahimi S, Sadeghi-Bazargani H. Health care managers’ perspectives on the sources of evidence in evidence-based hospital management: A qualitative study in Iran. Ethiop J Health Sci [Internet]. 2017;27(6):659–68. Available from: https://www.ajol.info/index.php/ejhs/article/view/162555
Spiri WC, Kurcgant P, Pereira MV. Perception Of Nursing Middle Managers About The Evidence-Based Management. Int Arch Med [Internet]. 2017;10(February):11. Available from: http://imedicalsociety.org/ojs/index.php/iam/article/view/2311
Harris C, Allen K, Waller C, Green S, King R, Ramsey W, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 5: developing a model for evidence-driven resource allocation in a local healthcare setting. BMC Health Serv Res. 2017;17(1):1–18.
Belay T, Mbuya N, Rajan V. Data utilization and evidence-based decision making in the health sector: survey of three Indian states [Internet]. 2009 [cited 2018 May 26]. Available from: https://openknowledge.worldbank.org/handle/10986/3161
Niedzwiedzka BM. Barriers to evidence-based decision making among Polish healthcare managers. Heal Serv Manag Res [Internet]. 2003 May 21 [cited 2018 May 19];16(2):106–15. Available from: https://doi.org/10.1258/095148403321591429
Peirson L, Ciliska D, Dobbins M, Mowat D. Building capacity for evidence informed decision making in public health: A case study of organizational change. BMC Public Health [Internet]. 2012;12(1):137. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84857132983&doi=10.1186%2F1471-2458-12-137&partnerID=40&md5=68e18844316881fb3f2662477825d441
Buffett C, Ciliska D, Thomas H. Can I Use This Evidence in my Program Decision? Assessing Applicability and Transferability of Evidence. National Collaborating Centre for Methods and Tools (NCCMT) School of Nursing, McMaster University. 2007:1–22.
Buffet C, Ciliska D, Thomas H. It worked there. Will it work here? A tool for assessing applicability and transferability of evidence (A: When considering starting a new program). National Collaborating Centre for Methods and Tools (NCCMT) School of Nursing, McMaster University. 2011;(905):1–2.
Dobbins M, Jack S, Thomas H, Kothari A. Public health decision-makers’ informational needs and preferences for receiving research evidence. Worldviews Evidence-Based Nurs. 2007;4(3):156–63.
Wright AL, Zammuto RF, Liesch PW, Middleton S, Hibbert P, Burke J, et al. Evidence-based Management in Practice: Opening up the Decision Process, Decision-maker and Context. Br J Manag [Internet]. 2016 Jan [cited 2018 May 28];27(1):161–78. Available from: https://doi.org/10.1111/1467-8551.12123
Imani-Nasab MH, Seyedin H, Yazdizadeh B, Majdzadeh R. A Qualitative Assessment of the Evidence Utilization for Health Policy-Making on the Basis of SUPPORT Tools in a Developing Country. Int J Heal Policy Manag. 2017;6(8):457–65.
Lavis JN, Paulsen EJ, Oxman AD, Moynihan R. Evidence-informed health policy 2-Survey of organizations that support the use of research evidence. Implement Sci. 2008;3:54.
Bastani P, Kavosi Z, Alipoori S, Imani-Nasab MH. Evidence- based Policy and Decision-Making among Health Managers: A Case of Shiraz Univer- sity of Medical Sciences. GMJ. 2017;6(1):30–8.
Greaves DE. Evidence-based management of Caribbean health systems: barriers and opportunities. Int J Health Governance. 2017;22(2):104–117.
Acknowledgements
This research, derived from Proposal No. 96-01-07-14184, was conducted by Mrs. Tahereh Shafaghat as part of the activities required for a Ph.D. degree in health care management at the Shiraz University of Medical Sciences. The authors wish to express their sincere gratitude to the research administration of Shiraz University of Medical Sciences for its financial and administrative support and to the English editorial board of Research Editor Institution for improving the native English language of this work.
Funding
As the overall study was an approved research project of Shiraz University of Medical Sciences and it was conducted by Mrs. Tahereh Shafaghat as part of the activities required for a Ph.D. degree in the health care management field, the Shiraz University of Medical Sciences supported this study. This study was sponsored by Shiraz University of Medical Sciences under code (96‑01‑07‑14184). The funding body was not involved in the design of the study, data collection, analysis, and interpretation, as well as in writing the manuscript.
Author information
Authors and Affiliations
Contributions
PB and TSH designed the study and its overall methodology. BP also edited and finalized the article. TSH searched all the databases, with the help of MRAM retrieved the sources, scanned, and screened all the articles in 3 phases. TSH also prepared the draft of the article. MAB and MKRZ contributed to data analysis and synthesis. Also, the study was under consultation and supervision by ZK and MHIN as advisors. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Since at this study a scoping review was conducted and then the best-fit framework synthesis was used for developing a comprehensive EBDM framework in HSM, there was no human or animal participant in this study. However, the overall research project related to this manuscript was approved by the medical ethics conceal of the research deputy of Shiraz University of Medical Sciences with approval number IR.SUMS.REC.1396–01-07–14184.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shafaghat, T., Bastani, P., Nasab, M.H.I. et al. A framework of evidence-based decision-making in health system management: a best-fit framework synthesis. Arch Public Health 80, 96 (2022). https://doi.org/10.1186/s13690-022-00843-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-022-00843-0