- Systematic Review
- Open access
- Published:
Overview of the role of robots in upper limb disabilities rehabilitation: a scoping review
Archives of Public Health volume 81, Article number: 84 (2023)
Abstract
Background
Neuromotor rehabilitation and improvement of upper limb functions are necessary to improve the life quality of patients who have experienced injuries or have pathological outcomes. Modern approaches, such as robotic-assisted rehabilitation can help to improve rehabilitation processes and thus improve upper limb functions. Therefore, the aim of this study was to investigate the role of robots in upper limb disability improvement and rehabilitation.
Methods
This scoping review was conducted by search in PubMed, Web of Science, Scopus, and IEEE (January 2012– February 2022). Articles related to upper limb rehabilitation robots were selected. The methodological quality of all the included studies will be appraised using the Mixed Methods Appraisal Tool (MMAT). We used an 18-field data extraction form to extract data from articles and extracted the information such as study year, country, type of study, purpose, illness or accident leading to disability, level of disability, assistive technologies, number of participants in the study, sex, age, rehabilitated part of the upper limb using a robot, duration and frequency of treatment, methods of performing rehabilitation exercises, type of evaluation, number of participants in the evaluation process, duration of intervention, study outcomes, and study conclusions. The selection of articles and data extraction was made by three authors based on inclusion and exclusion criteria. Disagreements were resolved through consultation with the fifth author. Inclusion criteria were articles involving upper limb rehabilitation robots, articles about upper limb disability caused by any illness or injury, and articles published in English. Also, articles involving other than upper limb rehabilitation robots, robots related to rehabilitation of diseases other than upper limb, systematic reviews, reviews, and meta-analyses, books, book chapters, letters to the editor, and conference papers were also excluded. Descriptive statistics methods (frequency and percentage) were used to analyses the data.
Results
We finally included 55 relevant articles. Most of the studies were done in Italy (33.82%). Most robots were used to rehabilitate stroke patients (80%). About 60.52% of the studies used games and virtual reality rehabilitate the upper limb disabilities using robots. Among the 14 types of applied evaluation methods, “evaluation and measurement of upper limb function and dexterity” was the most applied evaluation method. “Improvement in musculoskeletal functions”, “no adverse effect on patients”, and “Safe and reliable treatment” were the most cited outcomes, respectively.
Conclusions
Our findings show that robots can improve musculoskeletal functions (musculoskeletal strength, sensation, perception, vibration, muscle coordination, less spasticity, flexibility, and range of motion) and empower people by providing a variety of rehabilitation capabilities.
Introduction
Impaired upper limb (UL) functions to restrict the performance of activities of daily living, limit social participation [1], specifically decrease the independence of affected individuals and reduce patients’ quality of life [2, 3]. In upper limb disabilities, patients develop musculoskeletal problems such as paresis, pain, loss of sensation, and spasticity in different parts of the upper limb and so these problems can have manifold consequences in the daily lives of those impacted. These include a decreased capacity to carry out primary self-care tasks and to accomplish life-roles, which can affect emotional, mental, and psychological wellbeing [4]. Patients with upper limb disabilities need rehabilitation to improve their musculoskeletal status [5].
Neuromotor rehabilitation and recovery of upper extremity functions are necessary to improve the life quality of individuals who have suffered injuries, disabilities or have pathological outcomes, where it is favorable to raise the development of activities of daily living [6]. However, the conventional rehabilitations done by one manual-assisted movement training created by physiotherapists suffers from a lot of inherent restrictions, such as heavy labor severity, long-time consumption, lack of repeatability, low patients participation, and their low motivation to perform rehabilitation exercises [7]. Also, in conventional therapy, the accessibility of therapists, the duration of therapy sessions, and the high cost of rehabilitation tools are all considered parameters that impact on both therapists and patients [8].
New therapeutic methods have been presented to rehabilitate and improve upper limb function, and such methods are robotic rehabilitation [1]. Severe repetitions of harmonized motor activities by robots establish an important burden for the therapists who help patients. Moreover and due to economic reasons, the duration of preliminary rehabilitation is getting shorter and shorter [9]. However, some studies have pointed out that repetitive and high-severity exercises can specifically contribute to the functional recovery of the affected upper limb movement [10]. Rehabilitation robots are able of decreasing the burden on therapists by replace human intervention and preparing desire therapies that accomplish the following primary principles of upper limb rehabilitation: iteration, high severity, and task particularly [11]. Moreover, the functional impetus of a patient can be activated to raise strenuous participation and improve cognitive functions. The physical factors and treatment data can be stored and analyzed by the sensing system, and that can provide a realistic basis for optimization training technique and speed up the recovery process [7]. In addition, major boost has been given by the extension of such devices to clinical care medical and rehabilitation centers [1, 2].
Therefore, multiple benefits can be considered for rehabilitation robots : they can produce high-quality repetitive movements and increase rehabilitation strength and intensity; they can offer many types of exercises for therapists to choose from; they supply a man-machine interaction that allows for objective measurement of advancement, which itself can status modifications in interaction by changing control parameters [12]. On the other hand, task-oriented training is one of the other capabilities of rehabilitation robots, which is known as the dominant and most effective method for motor rehabilitation of upper limb function [13]. Task-based approaches in which the patient is assisted to perform a specific prescribed movement, such as lifting an object with the hand, show promising results compared to conventional exercises based on passive movement of the impaired joints in the restriction of their range of motion [14].
Robots can also be used in homes, clinics and medical centers. Patients can do the rehabilitation exercises prescribed by the therapist with the help of the robot at home without having to visit the treatment center frequently. Successful robot-assisted rehabilitation at home can facilitate intensive therapy, facilitate in-person or virtual therapy visits, preferably at low cost, and motivate patients to participate in supervised or unsupervised therapeutic activities at necessary levels for motor learning and generalization to occur [15]. Moreover, in clinics, rehabilitation robots can decrease the burden of therapists by automating tedious and labor-intensive treatment and by adapting to the particularized needs of targeted individuals [16]. For example, the hand robot skeleton designed by Wege et al., [17] can move patients’ fingers skillfully and repeatedly compared to a tired therapist training patients with manual labor.
To our knowledge, no systematic or scoping review has been performed on robots to rehabilitate upper limb disabilities. Only a few systematic reviews have been done in the areas of classification of interactive wearable systems for monitoring body movement and posture during upper body rehabilitation, estimating the wearability of the wearable devices [18], presenting state of the art in sensor fusion applied in applications for hand rehabilitation [19], evaluating the role of serious games in upper limb rehabilitation, identifying common procedures and exercises as well as technology patterns [20], evaluating the effectiveness of upper limb wearable technology to improve activity and engagement in stroke survivors [21] and determining the effects of robot-assisted treatment on motor-functional improvement in stroke patients [22]. So, the aim of the present study was to investigate the role of robots in upper limb disability improvement and rehabilitation. In this study, we identify the most common diseases or complications leading to upper limb disability for which robots have been used for rehabilitation. Moreover, we identify the most important technologies that can be used along with rehabilitation robots, the types of evaluation methods of rehabilitation robots and the outcomes of robot use for individuals with upper limb disabilities.
Materials and methods
In the current study, we used the PRISMA scoping reviews checklist for selecting studies and reporting the results [23].
Search strategy and information sources
To find articles related to the rehabilitation of upper limb disabilities using robots, four databases, PubMed, Web of Science, Scopus, and IEEE were searched. In order to search these databases, the keywords related to the upper limb, rehabilitation, and robots were used. Relevant Medical Subject Heading (MeSH) Keywords, spelling differences and synonyms were included and altered as suitable for each database. Then, the below search strategy was developed by KB, ASH, and KHM and finally approved by AH.
((upper extremity disability OR upper limb disability) AND (rehabilitation OR telerehabilitation) AND (robot OR robotics))
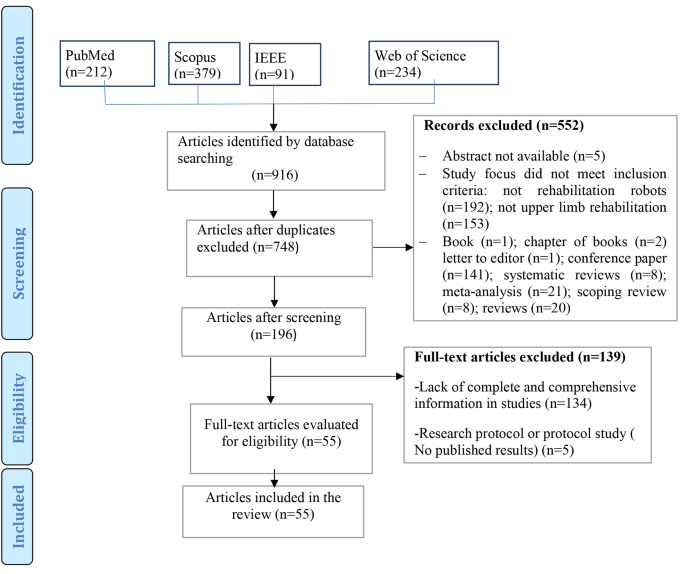
Articles addressing upper limb rehabilitation robots were included in to study. The PRISMA diagram is demonstrated in Fig. 1.
Eligibility criteria
Inclusion and exclusion criteria are presented below.
Inclusion criteria
-
1.
Articles involving upper limb rehabilitation robots.
-
2.
Articles about upper limb disability caused by any illness or injury.
-
3.
Studies involving rehabilitation robots designed for all ages.
-
4.
Robotic devices used with any assistive technologies (such as telerehabilitation systems and games based on virtual reality, etc.)
-
5.
Articles published in English.
-
6.
Time of publication between January 2012– February 2022.
It should be noted due to the rapid development of technologies and rehabilitation robots, we limited our investigation to the last ten years. We wanted to identify the latest and newest technologies that can be used along with rehabilitation robots, evaluation methods and the outcomes of these robots in recent years. Xue et al. [24], believed that rehabilitation robotics is a relatively young field growing rapidly with increasing penetration into therapeutic environments. Therefore, the newer dimensions of this rehabilitation tool should always be considered. In addition, the number of articles published in the last ten years was sufficient to answer the questions of this research. Therefore, this scoping review included articles published from January 2012– February 2022.
Exclusion criteria
-
1.
Articles involving other than upper limb rehabilitation robots.
-
2.
Robots related to rehabilitation of diseases other than upper limb.
-
3.
Systematic reviews, reviews, and meta-analysis.
-
4.
Books.
-
5.
Book chapters.
-
6.
Letter to the editor.
-
7.
Conference abstracts.
-
8.
Research protocol or protocol study.
Study selection
First, abstracts of all related articles were retrieved from four databases: PubMed, Web of Science, Scopus, and IEEE, and imported into EndNote software by KHM. Duplicate articles were removed. After studying the title, and abstract, the relevant articles were selected according to the inclusion and exclusion criteria by KHM and ASH. Then, all studies included in the study were reviewed and finalized by KB and AH. In disagreement, the final decision on each article is decided by discussion among the study team members. Finally, the full text of the articles was studied to extract data and information from KHM and ASH.
Critical appraisal of individual sources of evidence
Critical evaluation of data was done by ASH and KHM independently using Mixed Methods Appraisal Tool (MMAT, version 2018: Hong et al., 2018). Disagreement between authors (n = 4 articles) was resolved by discussion between two other authors (KB and AH) until reaching an agreement. We evaluated studies according to the MMAT criteria according to the selected category. The latest version of the MMAT offers a descriptive quality appraisal instead of a summative numerical score. Answer options in all study categories include “yes”, “no” and “can’t tell”. The answer “can’t tell” indicates that not enough information was reported in the study for a “yes” or “no” answer. A “can’t tell” rating may indicate a need to search for companion studies or contact study authors for more information [25].
Data charting process and data items
Data were extracted using a predetermined form. The validity of this form was confirmed by two specialists in medical informatics and software engineer, a physiotherapist, and a specialist in health information management. This data extraction form also includes fields such as year, country, type of study, purpose, illness or accident leading to disability (Table 1), level of disability (Table 2), assistive technologies (telerehabilitation, virtual reality or games) (Table 1 and more details in Appendix B), number of participants in the study, sex, age (Table 3 and more details in B)), rehabilitated part of the upper limb using a robot (Table 4), duration and frequency of treatment, methods of performing rehabilitation exercises, type of evaluation, number of participants in the evaluation process (Table 5 and more details in Appendix B), study outcomes (Table 6 and more details in Appendix B) and study conclusions (more details in Appendix B).
Data collation process
The information extracted from the articles was re-examined by KB and finally approved by AH. In case of disagreement, the consensus was achieved by the review of the members of the study team. It should be noted that for articles with missing data and information, we emailed the corresponding author and asked them to send us the necessary information. Finally, two authors extracted all data from eligible full-text documents through Excel.
Synthesis of results
After the data were stored and managed in MS Excel for processing, to synthesize data, one author (KHM) checks all imported data (e.g., spell check, cell formatting). Then, descriptive statistics (frequency and percentage) were used to summarize the collected data. Descriptive data obtained from the findings of the included articles were organized into tables and figures based on themes to present the findings of this review, which guided the study aims by (KB, AH, and ASH).
Ethical considerations
The protocol of this study was approved by the ethical committee of Kerman University of Medical Sciences) IR.KMU.REC.1400.606).
Results
Study selection process
From the 348 non-duplicate articles found using the search strategy, 55 articles were selected for inclusion (Fig. 1). Summarized findings from selected articles are included in Table 1.
Critical appraisal of individual sources of evidence
The findings of the quality assessment of studies based on MMAT are presented in Appendix A.
Results of the reviewed studies
Most of the studies were done in Italy (n = 19, 34.55%) [26,27,28, 31, 33, 36, 37, 43, 46,47,48,49, 57, 62, 63, 68, 76, 79]. After Italy, 14.24% and 8.9% of the studies were conducted in the USA (n = 8) [29, 42, 50, 51, 56, 60, 61, 72] and China (n = 5) [32, 54, 59, 65, 73], respectively. (More details in Table 1). Also, most of the studies were RCT (n = 26) [28,29,30,31, 35, 36, 40,41,42, 47, 48, 50, 53,54,55, 63, 66, 68, 70, 72, 73, 75, 76, 78,79,80].
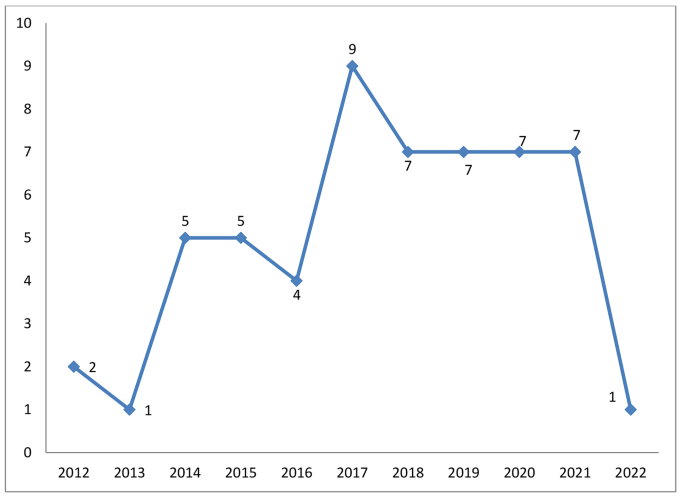
As shown in Fig. 2, most articles on robots for upper limb rehabilitation were published in 2017 (n = 9) [33,34,35, 60, 61, 67, 72, 79, 80], 2020 (n = 7) [46,47,48,49,50, 63, 64, 69], and 2021 (n = 7) [51,52,53,54,55, 65, 73]. (More details in Table 1)
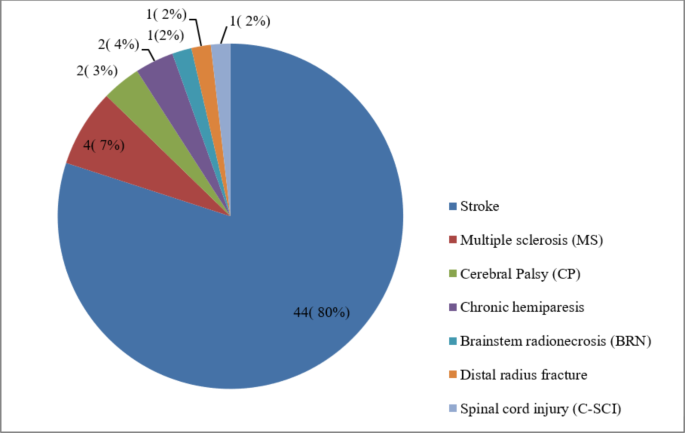
Robots were used to rehabilitate seven categories of diseases or complications leading to upper limb disability (Fig. 3). Most robots were used for patients with stroke (n = 44, 80%) [28, 29, 31,32,33,34,35, 37,38,39,40,41,42, 44, 45, 48,49,50,51,52,53,54,55,56,57,58,59,60,61,62, 64,65,66, 68, 70, 72,73,74,75,76,77,78,79,80]. Other diseases with frequencies and percentages are shown in Fig. 3.
Eight different levels of upper limb disability were identified (Table 2). The highest frequency of disabilities was related to the entire upper limb (n = 30). Wrist (n = 10), fingers (n = 7) and arm (n = 7) were other parts of the upper limb that had the highest level of disabilities. (More details in Table 1)
Table 4 shows that some robots were designed to be used to rehabilitate the entire upper limb (n = 15). Then, robots were mostly used for wrist (n = 14), finger (n = 12), and shoulder (n = 11) rehabilitation, respectively. (More details in Appendix B)
Use of telerehabilitation and virtual reality in robots.
60.52% of the studies used games and virtual reality to rehabilitate the upper extremities in robots [26, 30,31,32, 36, 38, 40, 42,43,44,45,46,47,48,49,50,51, 54, 55, 57, 59,60,61,62, 64, 66,67,68,69,70,71,72,73, 75](n = 34). Moreover, 3.56% of studies had used telerehabilitation in their robots (n = 2) [32, 35].
Evaluations in upper limb rehabilitation robots
The number of participants in the evaluation of upper limb rehabilitation robots varied from one [43, 46, 59, 64, 77] to 224 [48]. According to Tables 3, 89% of the studies used both males and females in the robot evaluation process(n = 49) [26,27,28,29, 31,32,33,34,35,36,37,38,39,40,41,42, 44, 45, 47,48,49,50,51,52,53,54,55,56,57,58, 60,61,62,63, 65,66,67,68,69,70,71,72,73,74,75,76, 78,79,80]. Most of the participants were over 18 years old (n = 47, 85%) [26,27,28,29, 31, 33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51, 53,54,55,56,57,58,59,60, 62, 63, 65,66,67,68, 70,71,72,73, 75, 78,79,80]. Moreover, in some studies, the age of the participants was less than or equal to 18 years (n = 4, 7%) [30, 67, 69, 76]. The minimum and maximum duration of evaluation processes were 30–45 min [26] to 12 months [52], respectively. Also, 83% of the studies included both male and female patients in the robot evaluation process. One study included only women [43], and two studies focused on men [46, 77] (More details in Appendix B).
The duration of treatment of patients in 38% of studies was less than one month (n = 21) [26, 28, 32, 33, 35, 39, 47, 49, 51, 54, 56, 58, 60, 62,63,64, 66, 68, 72, 73, 75]. In 41% of the studies (n = 23) [29,30,31, 34, 36, 40, 43,44,45,46, 50, 53, 55, 57, 61, 65, 67, 69, 71, 76, 78,79,80], the duration of treatment of patients was between one and two months. In other studies, the duration of treatment of patients was more than three months [27, 42, 48, 52, 70](n = 5, 9%) (More details in Appendix B).
According to Tables 5, 14 types of evaluation were performed for upper limb rehabilitation robots. “Evaluation and measurement of upper limb function and dexterity” was the most common type of evaluation (n = 52). “Range and motor skills and functional strength of the hand” were ranked next (n = 12). Then, “Neuropsychological assessment” was the most common type of evaluation (n = 11). As shown in Tables 5, 85 different evaluation methods were used. “Fugl-Meyer Upper Extremity score” was the most used evaluation method in studies (n = 30). Then, “Barthel Index (BI)” (n = 11), “Modified Ashworth Scale (MAS)” (n = 11), and “Box and Block Test (BBT)” (n = 11) were the most widely used evaluation methods.
Outcomes of using upper limb rehabilitation robots
The most important outcomes of upper limb rehabilitation robots were “Improvement in musculoskeletal functions”, “No adverse effect on patients”, and “Safe and reliable treatment”, respectively. Other outcomes are listed in Table 6. (More details in Appendix B).
Discussion
In this scoping review, outcomes of rehabilitation robots for upper limb disabilities and different methods for evaluating rehabilitation robots were identified. Most robots were used for the rehabilitation of patients with stroke. Along with robots, telerehabilitation and virtual reality, technologies were also used for upper limb disabilities rehabilitation. “Evaluation and measurement of upper limb function and dexterity” was the most common type of evaluation among the 14 types performed for upper limb rehabilitation robots. Also, we identified different outcomes of using rehabilitation robots for upper limb disabilities.
As discussed above, telerehabilitation and virtual reality were two types of technology used along with rehabilitation robots. Some studies [3, 82, 83] showed that if special interventions such as game-based virtual reality, and telerehabilitation with rehabilitation robots are used, upper limb function, mental health and patients’ participation in rehabilitation exercises can be improved. Moulaei et al. [3], showed in a scoping review that telerehabilitation could lead to “improving in musculoskeletal functions”, “increasing patients’ interest and motivation to perform rehabilitation exercises”, “increasing adherence to rehabilitation exercises and more participation in treatment processes”, “remote monitoring and control of patients”, “reducing or relieved pain” and “improving quality of life”. Fernández-Vázquez et al. [84], also pointed out that virtual reality as a very interesting tool in treating upper limb disorders along with rehabilitation robots can improve the motor function of the upper limb, increase users’ motivation and enjoyment, a large number of repetitions or high intensity rehabilitation. Repetitive and long exercises become easy and reduce the time needed to perform therapeutic exercises. Some studies [85,86,87] stated that for telerehabilitation systems and virtual reality to be as effective as robots, they should be easy to use, user-friendly, and have a beautiful and appropriate user interface. Zanatta et al. [87] pointed out that when telerehabilitation systems, robots and virtual reality are usable and attractive, patients’ motivation to perform rehabilitation exercises increases, their satisfaction with treatment processes increases, and efficiency and effectiveness increase. Therefore, to combine the robot with telerehabilitation or virtual reality to be effective, various factors such as usability, suitable user interface and even technical support should be considered in design, development and implementation.
The findings of this study and other reviews [2, 22, 88, 89] have shown that rehabilitation robots have been able to improve the musculoskeletal status of patients with upper limb disabilities. FMA-UE scores obtained from different studies showed that robot-based treatments can improve upper limb musculoskeletal function [1, 90,91,92]. In a review of the literature on therapeutic robotics in chronic stroke survivors and individuals with hemiparesis, the FMA total score improved from 2.1 to 15.1 and the ARAT improved to 11.1 [1, 90,91,92]. Milot et al. [91], tested 20 volunteers with mild to moderate chronic stroke to investigate the robot’s functional outcomes on the upper limb. Their study showed that training with the robot led to significant improvements in FMA, BBT, MAL, WMFT, and quantitative amounts of strength and speed, and these statuses were maintained in the 3-month follow-up [91]. Cimolin et al., [93] conducted a clinical trial using the Armeo Spring device on children aged 4 to 17 years with cerebral palsy. The subjects of this study showed promising improvements in different movement patterns and hand functions. It seems that to increase the effect of robots on improving upper limb disabilities, it is better to consider a number of factors. For example, the mechanical characteristics of rehabilitation robots may affect outcomes. Exoskeleton robots can control several joints simultaneously, leading to tight physical interaction between humans and robots, which may increase the patient burden.
Additionally, the exoskeleton robot’s high inertia to its complex structure can intervene with manipulation. Or, in the mechanical dimensions of the robot, the degree of freedom should be considered an important factor in the design. For example, intervention with six degrees of freedom in a three-dimensional space is very challenging for stroke patients with moderate to severe motor impairment [1]. The term “paradox of reduced number of degrees of freedom” states that to train a patient with a severe movement disorder, one should first use the lowest number of degrees of freedom, then gradually increase the number of degrees of freedom as improvements are achieved [94]. On the other hand, if the robots are not light, they can put pressure on different organs of patients during exercise. Also, rehabilitation robots can be costly, except for people who might profit from using them for training. As a result, efforts should be made to make rehabilitation robots as cost-effective as possible. Finally, these devices should be easily available to people, and awareness of them as an effective and helpful alternative treatment should also continuously increase.
Although, in this review we observed that rehabilitation robots have no adverse effect on patients, in some studies, the complications of rehabilitation robots have been mentioned [89]. Bessler et al. [95], believed that the safety of using rehabilitation robots in clinical trials should be confirmed for monitoring and reporting adverse events. In a systematic literature review, Bessler et al. [89], gathered information on the type of adverse events associated with the training of static robotic gait trainers. They identified about 17 adverse events per 100 people trained on a stationary robotic gait trainer. The most common types of side effects were classified into two categories: side effects related to soft tissue and musculoskeletal side effects. The third category included physiological adverse events (such as sudden changes in blood pressure) that seem to be unrelated to the mechanical settings of the robotic device in most cases, but are generally considered to be related to the activity engaged. Side effects associated to soft tissue in trainers also included things such as skin redness, skin irritation, open skin lesions and bruising, skin abrasion, as well as hurt and pain in soft tissue areas. Musculoskeletal side effects also included tendinopathy, muscle pain, tibial fracture, back and malleolus pain, and joint discomfort and pain [89]. Therefore, rehabilitation robots should be designed to minimize the side effects related to all three dimensions, i.e., soft tissue, musculoskeletal, and physiological. First of all, it can be said that the designers of these systems must ensure that there are no side effects before using robots by patients or therapists, so that they can be used safely for rehabilitation. Then, the therapists should set the rehabilitation exercises in terms of dosage and duration in such a way that the side effects caused by the low or high use of the robot do not occur for the patients.
Besides, we should be able to improve the design, development and evaluation of rehabilitation robots so that they have the necessary quality to provide rehabilitation services. Abu-Dakka et al. [96] believed that rehabilitation robots should be designed in a way that can be easily used by patients, therapists, and clinicians, increase the effectiveness of doctors’ treatments and make patients’ daily activities easier. To achieve these goals, rehabilitation robots must have some functional requirements, including: stability, safety, adaptability to patient needs, accept a wide range of patients, providing a full Range of Motion (ROM), being equipped with the necessary sensors for haptic and visual feedback, etc. [97, 98]. Also, in the design and evaluation of rehabilitation robots, we must consider the views and opinions of users (patients and therapists), because these people are the end users of these rehabilitation tools. Considering the perspectives and opinions of patients and therapists in the design process also makes the device develop according to the patients’ needs and preferences. As a result, their level of satisfaction and continued use of this device improves. Zanatta et al., [87] believed that considering the patient’s perspective when designing or evaluating a rehabilitation device is essential to ensure adequate engagement and adherence to treatment. Or when the usability of a rehabilitation robot is suitable for users, according to Nielsen [99], learnability, efficiency, memorability and satisfaction of users improve, while the rate of errors also decreases.
Accordingly, a patient who perceives a device as usable is likely also report a positive perception as a concern: ease of learning the system’s function and behavior, effort expended to reach a goal, ease of remembering the system’s performance for any further use, the system’s ability to easily support and recover the case of errors during use and the pleasant design of the system. Thus, assessing such aspects provides important insights into the acceptability and perceived usefulness of devices, thereby allowing an understanding of how to improve patient motivation during treatment. As emphasized in Monardo’s study [100], motivation plays an essential role during the rehabilitation process because it helps create a sense of patient competence and satisfaction. In addition, patient satisfaction with treatment-rehabilitation processes performed with the help of rehabilitation devices was associated with stronger treatment compliance [101]. As a result, both factors can be considered key factors for the effectiveness of treatment-rehabilitation processes. On the other hand, the anatomical structure of the upper limb, the severity and degree of the patients’ disabilities, and the age group of the patients (for example, children or the elderly) should also be considered when designing and developing a rehabilitation tool. For example, a rehabilitation robot may only be used by children and not by elderly persons [102] or a robot may be designed for finger rehabilitation-only [103].
According to the findings of the studies, we found that robots were a safe and reliable treatment for patients. Therefore, it is necessary to consider a set of factors for the rehabilitation robot to guarantee patient safety and maintain its reliability for patients. Sampson et al. [104], evaluated the BUiLT + VR system in hemiparetic patients with upper extremity disability and found that this system is reliable for treating patients and can be administered safely. They believed that through Rests between games, ramping of the time spent playing in the early sessions, and adjustments to seating, unit height and angle, it could overcome the challenges related to patient safety and increase its reliability for users. Other studies show that the designed rehabilitation robot should ensure the safety of the patients from the aspects of using the common sensor to monitor and manage the force information of the patients during movement, when the reaction force made by the muscle tension is very high. Also, when the patient experiences a muscle spasm, the robot should automatically stop the current movement so that the muscle is not strained. Therefore, to prevent repeated injury to patients, the space and working environment should be restricted by limiting the switch within a reasonable range. The rehabilitation robot’s speed of displacement and movement should also be limited by the software used to control the robot. The operator or therapists should be able to rationally adjust the parameters of the driving device, and control and monitor the movement status of the robot in real time. Pressing the stop button is very important to avoid accidents. Also, to avoid damage created by the rotation of the joints due to gravity, the rehabilitation robot’s ability to self-lock should be considered [105].
Reduction or relief of pain was another outcome of this review. Some studies [75, 95] have shown that robots can reduce or relieve pain in patients, but factors must be considered when designing or using robots so that the robot can reduce pain more effectively. For example, exceeding forces on the human musculoskeletal system, at the same time misalignment will make high pressure and shear forces via slipping at the cuffs or straps [106, 107]. Therefore, forces that are not considered or compensated for in the design of the robot or its interface are easily transmitted to the musculoskeletal systems. On the other hand, if the torques and forces are too high or act in arbitrary directions on the musculoskeletal system, they can create an additional load, resulting in pain and damage to the bones, joints, and muscles [95, 106]. Therefore, when designing robots, pain thresholds should be considered for pressures and forces applied during accidental contact such as collisions or closing situations with a robot [108]. Different limit values for many different parts of the human body are accepted by ISO/TS 15,066 [95]. The patient’s position to perform therapeutic exercises with the help of the robot is also very effective in reducing pain. The robot developed in Kim et al.‘s [75] study allows patients to be comfortable and supported in a supine position. This way can easily be linked to other pain therapeutic methods, such as interferential current therapy or hot pack application. For example, installing a friction plate to forbid the compensation of the scapula and to increase the therapy’s effectiveness and adjust the robotic arm’s height using a linear actuator can be very helpful [75].
Duration and intensity of the therapy through the robot are two other factors that effect on the robots in motor control and improving pains. By examining the effectiveness of robots on function and structure in patients with limited upper limb function, Ferreira et al., [109] showed that when robot-assisted therapy is used with conventional treatment at the same dose and duration, robot-assisted therapy has a significant effect motor control. The group’s analysis also proposed an effect of the number of sessions and duration of treatment on some estimated impacts. The greater number of sessions and the volume of treatment affect motor control [109]. The more significant treatment dose effect was proposed by Lohse et al. [110]; however, time as a representation of dose is a rather rough estimate and supplies no evidence of the actual amount of movement or types of movement, nor does it account for periods of inactivity or rest [111]. In this respect, a previous study showed that, although there is no agreement, the minimum dose should be at least 16 h of exercise [112]. Poor methodological quality and lower dose and duration of treatment may negatively affect the estimated effects. So, therapists usually consider this approach because it has very few or no side effects [109]. Moreover, some studies have shown that low or high intensity exercise therapy can increase the risk of injury and worsening pain in the hemiplegic shoulder [113]. In the study by Kim et al. [75], participants in the intervention or control groups performed stretching exercises for 30 min per day, five times per week for four weeks; Shoulder pain in the intervention group (they used the robot) was worse than the control group. The authors of this research concluded that this stretching exercise was performed for patients with excessive intensity and more than 30 min of stretching exercise caused pain in some patients even when it was performed with low intensity.
As our study showed, robots can increase patients’ interest and motivation to perform rehabilitation exercises. Therefore, one of the other factors that can be considered to increase patients’ use of robots and their interest and motivation to perform rehabilitation exercises is the use of games and virtual reality. Creating a degree of entertainment through games and virtual reality can improve patients’ adherence to rehabilitation exercises and increase patients’ attention span to spend more time on their rehabilitation program [114]. Kafri et al. [115], investigated the effect of virtual reality on patients after a stroke. Patients showed an improvement in activity and reported that they enjoyed the game. Virtual reality also supplies direct visual feedback and can empower patients with a sense and awareness of control over their recovery. Consequently, it is imaginable that people who train with virtual reality and games will enhance their performance when interacting with an avatar presented on the screen [114]. In another study, Gomez et al., [116] evaluated patients with multiple sclerosis using games, in which the experimental group received both game sessions and conventional treatment. This study showed that after using the games, interest and motivation to perform rehabilitation exercises improved in the patients.
Efficiency and effectiveness of rehabilitation robots, increasing the patient’s independence in performing rehabilitation exercises, rehabilitation robots’ feasibility for training patients, performing repetitive and long exercises very easily with the help of the robot, reducing the duration of rehabilitation exercises, increasing adherence to rehabilitation exercises and more participation in treatment processes, and improving quality of life and rehabilitation process were other outcomes related to rehabilitation robots identified in this study. But it must be said that these outcomes or other mentioned outcomes will not be created spontaneously due to the use of rehabilitation robots, but a series of main factors or capabilities must be included in the robots so that these outcomes can be created and have a and beneficial effect in rehabilitation. For example, Laut et al. [117] believed that rehabilitation robots could potentially increase efficiency and access to treatment by having capabilities such as providing continuous training for a long period of time and collecting data to evaluate progress. Furthermore, by pairing rehabilitation robots with health information technologies and presenting assessment and performance data all over the internet to the therapist, different treatment processes can be moved out of specific facilities and into patients’ homes with remote management by a therapist. This can let a therapist treat several patients simultaneously, greatly enhancing the numbers of patients treated and the efficiency of the rehabilitation robot and therapist.
In other words, changing from a hospital to a home rehabilitation program can reduce costs while making rehabilitation more accessible [117]. Francisco et al. [118] also stated that by providing frequent and intensive training through rehabilitation robotics, the effectiveness of conventional occupational therapy or physiotherapy can be improved by providing more coherent, accurate, and precise treatment. Therefore, it should be said that for robots to be able to teach patients better or be more efficient, they must be able to provide frequent and intensive training. Also, in order to improve the efficiency and effectiveness of a rehabilitation device, the satisfaction of patients should be maximized. According to Tousignant et al.‘s study [119], satisfaction is an important indicator and factor for the degree of efficiency and effectiveness. Its high level can increase patient motivation, and adherence to treatment, and improve compliance with treatment. Also, it should be noted that satisfaction is one of the important factors in the quality of health care; it can affect adherence to treatment plans, improve clinical outcomes [120], and motivation of patients to perform rehabilitation exercises [121]. In order to maximize satisfaction, the robot must be designed according to the needs and preferences of its users, be usable and easy to use, and have no side effects [122, 123].
In addition, concerning adherence to rehabilitation exercises, it can be said that considering technologies such as sensors and computer game technologies for home rehabilitation or mRehab (mobile rehabilitation) systems in robots greatly increases the possibility of objective quantification of adherence [124]. Also, for patients to engage and be challenged while performing rehabilitation exercises at home in the physical absence of the therapist, there is a need to carefully design scenarios and motivational features that guarantee the patient’s adherence to the treatment plan [125]. Increasing the quality of life was another important outcome of using rehabilitation robots identified in our study. In the study by Kutner et al. [126], it was shown that patients who had suffered a stroke experienced a faster increase in quality of life (in physical, mental and social dimensions) after participating in targeted interventions that focused on improving upper limb strength. Mohammed et al. [127], in their study of patients with upper and lower limb amputation, defined the quality of life in three dimensions physical, mental and social health. Therefore, it should be said that when a rehabilitation robot is designed, in order to increase the quality of life of the patients, it should be focused on all three dimensions of the patients’ health, physical, psychological and social.
In general, it can be said that although the findings of the present study showed that rehabilitation robots could lead to positive outcomes for people with upper limb disabilities with various diseases or injuries, but if the factors that lead to these outcomes in If these robots are not considered, they will never have the necessary efficiency, effectiveness and quality.
Prospects of rehabilitation robots
It is predictable that rehabilitation robots will be applied much more than before in an era where the cost of manual therapy is becoming more expensive. To better popularize and commercialize this goal, future development needs to increase the universality of rehabilitation robots, focusing on portable, lightweight, reconfigurable, smart, and equipment based on artificial intelligence and machine learning techniques, new methods of treatment and thinking to the field of rehabilitation under the hypothesis of guaranteeing safety, mass production and development in a cheap direction [24]. For example, machine learning techniques may ,allow a robot to independently adapt to the changing needs of each customer over time and perform specific tasks, such as autonomous gaming [128]. Another example is the portability of the robot, which allows users to carry the robot system for deployment inside homes or medical centers [129]. People can use portable rehabilitation robots not only at home and in the treatment center, but also in nature and parks. On the other hand, Smart rehabilitation is the future development trend. It should be broken through the human-machine interface barrier, develop multidisciplinary and interdisciplinary collaboration and communication, improve and strengthen cooperation with rehabilitation medicine and artificial intelligence, actively participate in the design, development and evaluation of rehabilitation robots, and improve rehabilitation robots for providing better and more quality service to people.
Moreover, in the future, there should be more focus on “human nature” in the design and development of rehabilitation robots. Human nature means that robots have capabilities such as “perception, thinking, action and cooperation, expression and communication, and learning and adaptability and complete training and operations independently or with the assistance of an automatic machine” [24]. At present, rehabilitation robots cannot perform all the tasks of professional rehabilitation personnel; especially, the ability of self-learning, adaptability, flexibility and creativity of robots needs many theoretical developments. The most challenging and most difficult thing for rehabilitation robots is the benevolence and moral sense of medical staff [130]. Since in the future software packages and powerful hardware equipment will be produced, many of these problems can be easily solved.
Limitations of the study
There are a few limitations in this study. In the present study, only articles in English were reviewed; it is better to include articles published in non-English languages in future studies. Also, to find related studies, we searched four databases, Scopus, IEEE, PubMed, and Web of Science. It is suggested that more studies be done in more databases to obtain more comprehensive results.
Conclusion
This scoping review indicates that upper limb rehabilitation robots can improve musculoskeletal functions (Musculoskeletal strength, sensation, perception, vibration, muscle coordination, less spasticity, flexibility, and range of motion); avoid serious side effects or adverse effects on the patient, provide safe and reliable treatment, reduce pain, increase the patient’s independence in performing rehabilitation exercises, reduce the duration of rehabilitation exercises, increase adherence to rehabilitation exercises and treatment processes, and quality of life and rehabilitation processes. The use of rehabilitation robots is growing strongly, especially in developed countries, and it seems that this new rehabilitation technology has had significant effects in helping to improve upper limb disabilities.
Also, rehabilitation robots could provide a platform for motivating people with upper limb disabilities to carry out more rehabilitation exercises without a therapist, which could maximize recovery.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 9HPT:
-
Nine-Hole Peg Test
- AHA:
-
Assisting Hand Assessment
- AHF:
-
Arm-Hand Function
- AMAT:
-
Arm Motor Ability Test
- ARAT:
-
Action Research Arm Test
- BBT:
-
Box and Block Test
- BI:
-
Barthel Index
- BIT:
-
Behavioral Inattention Test
- BRN:
-
Brainstem radionecrosis
- C-SCI:
-
Spinal cord injury
- CBS:
-
Catherine Bergego Scale
- CEQ:
-
Credibility/Expectancy Questionnaire
- CP:
-
Cerebral Palsy
- DAS:
-
Disability Assessment Scale
- DASH:
-
Disabilities of Arm, Shoulder, and Hand
- DN4:
-
Douleur Neuropathique 4
- DSEMG:
-
Dynamic Surface Electromyography
- Euro-QOl:
-
Quality of Life
- FIM:
-
Functional Indipendence Measure
- FMA-UE:
-
Fugl-Meyer Upper Extremity score
- FMRI:
-
Functional magnetic resonance imaging
- fNIRS:
-
Functional near infrared spectroscopy
- GP:
-
Grooved Pegboard Test
- IMI:
-
Intrinsic Motivation Inventory
- JTHFT:
-
Jebsen-Taylor Hand Function Test
- K-SDQ:
-
Shoulder Disability Questionnaire
- MAL:
-
Motor Activity Log
- MAS:
-
Modified Ashworth Scale
- MAS:
-
Modified Ashworth Scale
- MCS:
-
Mental health Composite Score
- MeSH:
-
Medical Subject Heading
- MFT:
-
Manual Function Test
- MI:
-
Motricity Index
- MMSE:
-
Mini-Mental State Examination
- MRI:
-
Magnetic Resonance Imaging
- MRS:
-
Modified Rankin Scale
- MS:
-
Multiple sclerosis
- MSQOL-54:
-
Multiple Sclerosis Quality of Life-54
- NEADL:
-
Nottingham Extended Activities of Daily Living
- NIHSS:
-
National Institutes of Health Stroke Scale
- NRPS:
-
Numeric Rating Pain Scale
- NRS:
-
Numerical Rating Scale
- OCS:
-
Oxford Cognitive Screen
- PCS:
-
Physical health Composite Score
- PEDI:
-
Pediatric Evaluation of Disability Inventory
- POMA:
-
Performance Oriented Mobility Assessment
- PRWHE:
-
Patient-Rated Wrist and Hand Evaluation
- QOM:
-
Quality of Movement
- QUEST:
-
Quality of Upper Extremity Skills Test
- Quick-DASH:
-
Quick version of the Disabilities of the Arm, Shoulder, and Hand
- RCI:
-
Reliable Change Index
- RCT:
-
Randomized controlled trials
- ROCF:
-
Rey Osterrieth complex figure test
- ROM:
-
Active or Passive Range Of Motion
- SCWT:
-
Stroop Color and Word Test
- SDMT:
-
Symbol Digit Modalities Test
- SDMT:
-
Symbol Digit Modalities Test
- SDS:
-
Self-Depression Scale
- SF-36:
-
Short Form Health Survey
- SIS:
-
Stroke Impact Scale
- SIS:
-
Stroke Impact Scale
- TAM:
-
Total active mobility
- TMT:
-
Trail making test
- TSS:
-
Tremor Severity Scale
- UL:
-
Upper limb
- USE:
-
Usefulness, Satisfaction and Ease-of-use
- VAS:
-
Visual analog scale
- VAS:
-
Visual analogue scale
- WHODAS:
-
World Health Organization Disability Assessment Schedule
- WMFT:
-
Wolf Motor Function
References
Lee SH, Park G, Cho DY, Kim HY, Lee J-Y, Kim S, Park S-B, Shin J-H. Comparisons between end-effector and exoskeleton rehabilitation robots regarding upper extremity function among chronic stroke patients with moderate-to-severe upper limb impairment. Sci Rep. 2020;10(1):1806.
Vélez-Guerrero MA, Callejas-Cuervo M, Mazzoleni S. Artificial Intelligence-Based Wearable Robotic Exoskeletons for Upper Limb Rehabilitation: a review. Sens (Basel). 2021;21(6):2146.
Moulaei K, Sheikhtaheri A, Nezhad MS, Haghdoost A, Gheysari M, Bahaadinbeigy K. Telerehabilitation for upper limb disabilities: a scoping review on functions, outcomes, and evaluation methods. Archives of Public Health. 2022;80(1):196.
Poltawski L, Allison R, Briscoe S, Freeman J, Kilbride C, Neal D, Turton AJ, Dean SJD. rehabilitation: Assessing the impact of upper limb disability following stroke: a qualitative enquiry using internet-based personal accounts of stroke survivors. 2016, 38(10):945–51.
Maciejasz P, Eschweiler J, Gerlach-Hahn K, Jansen-Troy A, Leonhardt S. A survey on robotic devices for upper limb rehabilitation. J Neuroeng Rehabil. 2014;11(1):3.
Vélez-Guerrero MA, Callejas-Cuervo M, Mazzoleni S. Design, Development, and testing of an Intelligent Wearable Robotic Exoskeleton Prototype for Upper Limb Rehabilitation. Sens (Basel). 2021;21(16):5411.
Wu Q, Wu H. Development, dynamic modeling, and Multi-Modal Control of a therapeutic exoskeleton for Upper Limb Rehabilitation Training. Sens (Basel). 2018;18(11):3611.
Qassim HM, Wan Hasan WZ. A Review on Upper Limb Rehabilitation Robots. Appl Sci 2020, 10(19).
Richards L, Hanson C, Wellborn M, Sethi A. Driving motor recovery after stroke. Top Stroke Rehabil. 2008;15(5):397–411.
Qian Q, Nam C, Guo Z, Huang Y, Hu X, Ng SC, Zheng Y, Poon W. Distal versus proximal - an investigation on different supportive strategies by robots for upper limb rehabilitation after stroke: a randomized controlled trial. J Neuroeng Rehabil. 2019;16(1):64–4.
Langhorne P, Bernhardt J, Kwakkel GJTL. Stroke rehabilitation. 2011, 377(9778):1693–1702.
Qian Z, Bi ZJAiME. Recent development of rehabilitation robots. 2015, 7(2):563062.
Schweighofer N, Choi Y, Winstein C. Gordon JJAJoPM, Rehabilitation: Task-oriented rehabilitation robotics. 2012, 91(11):S270-S279.
Ennaiem F, Chaker A, Laribi MA, Sandoval J, Bennour S, Mlika A, Romdhane L, Zeghloul SJAS. Task-Based design approach: development of a planar cable-driven parallel robot for upper limb rehabilitation. 2021, 11(12):5635.
Johnson MJ, Loureiro RC, Harwin WSJISR. Collaborative tele-rehabilitation and robot-mediated therapy for stroke rehabilitation at home or clinic. 2008, 1(2):109–21.
Nizamis K, Athanasiou A, Almpani S, Dimitrousis C, Astaras AJS. Converging robotic technologies in targeted neural rehabilitation: A review of emerging solutions and challenges. 2021, 21(6):2084.
Wege A, Zimmermann A. Electromyography sensor based control for a hand exoskeleton. In: 2007 IEEE International Conference on Robotics and Biomimetics (ROBIO): 2007: IEEE; 2007: 1470–1475.
Wang Q, Markopoulos P, Yu B, Chen W, Timmermans A. Interactive wearable systems for upper body rehabilitation: a systematic review. J Neuroeng Rehabil. 2017;14(1):20.
Herrera-Luna I, Rechy-Ramirez EJ, Rios-Figueroa HV, Marin-Hernandez AJISJ. Sensor fusion used in applications for hand rehabilitation: A systematic review. 2019, 19(10):3581–3592.
Koutsiana E, Ladakis I, Fotopoulos D, Chytas A, Kilintzis V, Chouvarda I. Serious Gaming Technology in Upper Extremity Rehabilitation: scoping review. JMIR Serious Games. 2020;8(4):e19071–1.
Parker J, Powell L, Mawson S. Effectiveness of Upper Limb Wearable Technology for improving activity and participation in adult stroke survivors: systematic review. J Med Internet Res. 2020;22(1):e15981–1.
Kwakkel G, Kollen BJ, Krebs HIJN. repair n: Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. 2008, 22(2):111–21.
PRISMA for Scoping Reviews. [https://prisma-statement.org/Extensions/ScopingReviews].
Xue X, Yang X, Deng Z, Tu H, Kong D, Li N, Xu F. Global Trends and hotspots in Research on Rehabilitation Robots: a bibliometric analysis from 2010 to 2020. Front Public Health. 2021;9:806723.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F. Nicolau BJRoc: Mixed methods appraisal tool (MMAT), version 2018. 2018, 1148552(10).
Carpinella I, Cattaneo D, Bertoni R, Ferrarin M. Robot training of upper limb in multiple sclerosis: comparing protocols with or without manipulative task components. IEEE Trans neural Syst rehabilitation engineering: publication IEEE Eng Med Biology Soc. 2012;20(3):351–60.
Sale P, Bovolenta F, Agosti M, Clerici P, Franceschini M. Short-term and long-term outcomes of serial robotic training for improving upper limb function in chronic stroke. Int J rehabilitation Res Int Z fur Rehabilitationsforschung Revue Int de recherches de readaptation. 2014;37(1):67–73.
Pennati GV, Da Re C, Messineo I, Bonaiuti D. How could robotic training and botolinum toxin be combined in chronic post stroke upper limb spasticity? A pilot study. Eur J Phys Rehabil Med. 2015;51(4):381–7.
McCabe J, Monkiewicz M, Holcomb J, Pundik S, Daly JJ. Comparison of robotics, functional electrical stimulation, and motor learning methods for treatment of persistent upper extremity dysfunction after stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2015;96(6):981–90.
Gilliaux M, Renders A, Dispa D, Holvoet D, Sapin J, Dehez B, Detrembleur C, Lejeune TM, Stoquart G. Upper Limb Robot-Assisted therapy in cerebral palsy: a single-blind randomized controlled trial. Neurorehabilit Neural Repair. 2015;29(2):183–92.
Taveggia G, Borboni A, Salvi L, Mulé C, Fogliaresi S, Villafañe JH, Casale R. Efficacy of robot-assisted rehabilitation for the functional recovery of the upper limb in post-stroke patients: a randomized controlled study. Eur J Phys Rehabil Med. 2016;52(6):767–73.
Song AG, Wu CC, Ni DJ, Li HJ, Qin HY. One-therapist to three-patient Telerehabilitation Robot System for the Upper Limb after Stroke. Int J Social Robot. 2016;8(2):319–29.
Trujillo P, Mastropietro A, Scano A, Chiavenna A, Mrakic-Sposta S, Caimmi M, Molteni F, Rizzo G. Quantitative EEG for Predicting Upper Limb Motor Recovery in Chronic Stroke Robot-Assisted Rehabilitation. IEEE Trans Neural Syst Rehabil Eng. 2017;25(7):1058–67.
Saita K, Morishita T, Hyakutake K, Fukuda H, Shiota E, Sankai Y, Inoue T. Combined therapy using botulinum toxin A and single joint hybrid assistive limb for upper-limb disability due to spastic hemiplegia. J Neurol Sci. 2017;373:182–7.
Hsieh YW, Wu CY, Wang WE, Lin KC, Chang KC, Chen CC, Liu CT. Bilateral robotic priming before task-oriented approach in subacute stroke rehabilitation: a pilot randomized controlled trial. Clin Rehabil. 2017;31(2):225–33.
Gandolfi M, Vale N, Dimitrova EK, Mazzoleni S, Battini E, Benedetti MD, Gajofatto A, Ferraro F, Castelli M, Camin M et al. Effects of High-intensity Robot-assisted Hand Training on Upper Limb Recovery and Muscle Activity in Individuals With Multiple Sclerosis: A Randomized, Controlled, Single-Blinded Trial. Front Neurol 2018, 9.
Germanotta M, Cruciani A, Pecchioli C, Loreti S, Spedicato A, Meotti M, Mosca R, Speranza G, Cecchi F, Giannarelli G et al. Reliability, validity and discriminant ability of the instrumental indices provided by a novel planar robotic device for upper limb rehabilitation. J Neuroeng Rehabil 2018, 15.
Kim GW, Won YH, Seo JH, Ko MH, EFFECTS OF NEWLY DEVELOPED COMPACT ROBOT-AIDED UPPER EXTREMITY TRAINING SYSTEMS (NEURO-X. (R)) IN PATIENTS WITH STROKE: A PILOT STUDY. J Rehabil Med. 2018;50(7):607–12.
Iwamoto Y, Imura T, Suzukawa T, Fukuyama H, Ishii T, Taki S, Imada N, Shibukawa M, Inagawa T, Araki H, et al. Combination of Exoskeletal Upper Limb Robot and Occupational Therapy improve activities of Daily living function in Acute Stroke Patients. J stroke Cerebrovasc diseases: official J Natl Stroke Association. 2019;28(7):2018–25.
Dehem S, Gilliaux M, Stoquart G, Detrembleur C, Jacquemin G, Palumbo S, Frederick A, Lejeune T. Effectiveness of upper-limb robotic-assisted therapy in the early rehabilitation phase after stroke: a single-blind, randomised, controlled trial. Annals of Physical and Rehabilitation Medicine. 2019;62(5):313–20.
Hung CS, Lin KC, Chang WY, Huang WC, Chang YJ, Chen CL, Grace Yao K, Lee YY. Unilateral vs bilateral hybrid approaches for Upper Limb Rehabilitation in Chronic Stroke: a Randomized Controlled Trial. Arch Phys Med Rehabil. 2019;100(12):2225–32.
Conroy SS, Wittenberg GF, Krebs HI, Zhan M, Bever CT, Whitall J. Robot-Assisted arm training in chronic stroke: addition of transition-to-Task Practice. Neurorehabilit Neural Repair. 2019;33(9):751–61.
Bonanno L, Russo M, Bramanti A, Calabrò RS, Marino S. Functional connectivity in multiple sclerosis after robotic rehabilitative treatment: a case report. Medicine. 2019;98(17):e15047.
Leem MJ, Kim GS, Kim KH, Yi TI, Moon HI. Predictors of functional and motor outcomes following upper limb robot-assisted therapy after stroke. Int J rehabilitation Res Int Z fur Rehabilitationsforschung Revue Int de recherches de readaptation. 2019;42(3):223–8.
Kim DH, Kim KH, Lee SM. The effects of virtual reality training with Upper Limb sensory Exercise Stimulation on the AROM of Upper Limb joints, function, and concentration in chronic stroke patients. Phys Medizin Rehabilitationsmedizin Kurortmedizin. 2020;30(2):86–94.
Tartamella F, Chillura A, Pisano MF, Cacioppo A, Licari S, Caradonna D, Portaro S, Calabr RS, Bramanti P, Naro A. A case report on intensive, robot-assisted rehabilitation program for brainstem radionecrosis. Medicine 2020, 99(10).
Solaro C, Cattaneo D, Basteris A, Carpinella I, De Luca A, Mueller M, Bertoni R, Ferrarin M, Sanguineti V. Haptic vs sensorimotor training in the treatment of upper limb dysfunction in multiple sclerosis: A multi-center, randomised controlled trial. J Neurol Sci 2020, 412.
Aprile I, Germanotta M, Cruciani A, Pecchioli C, Loreti S, Papadopoulou D, Montesano A, Galeri S, Diverio M, Falsini C et al. Poststroke shoulder pain in subacute patients and its correlation with upper limb recovery after robotic or conventional treatment: A secondary analysis of a multicenter randomized controlled trial. Int J stroke: official J Int Stroke Soc 2020:1747493020937192.
Aprile I, Guardati G, Cipollini V, Papadopoulou D, Mastrorosa A, Castelli L, Monteleone S, Redolfi A, Galeri S, Germanotta M. Robotic Rehabilitation: An Opportunity to Improve Cognitive Functions in Subjects With Stroke. An Explorative Study. Front Neurol 2020, 11.
Kim GJ, Chen P. Role of instruction adherence during highly structured robotic arm training on Motor Outcomes for individuals after chronic stroke. Am J Phys Med Rehabil. 2020;99(4):353–6.
Bui KD, Wamsley CA, Shofer FS, Kolson DL, Johnson MJ. Robot-Based Assessment of HIV-Related Motor and Cognitive Impairment for Neurorehabilitation. IEEE Trans Neural Syst Rehabil Eng. 2021;29:576–86.
Flynn N, Froude E, Cooke D, Dennis J, Kuys S. The sustainability of upper limb robotic therapy for stroke survivors in an inpatient rehabilitation setting. Disabil Rehabil 2021.
Terranova TT, Simis M, Santos ACA, Alfieri FM, Imamura M, Fregni F, Battistella LR. Robot-Assisted Therapy and Constraint-Induced Movement Therapy for Motor Recovery in Stroke: Results From a Randomized Clinical Trial. Front Neurorobotics 2021, 15.
Qu QM, Lin YN, He ZJ, Fu JH, Zou F, Jiang ZW, Guo FX, Jia J. The Effect of Applying Robot-Assisted Task-Oriented Training Using Human-Robot Collaborative Interaction Force Control Technology on Upper Limb Function in Stroke Patients: Preliminary Findings. BioMed research international 2021, 2021.
Abd El-Kafy EM, Alshehri MA, El-Fiky AAR, Guermazi MA, Mahmoud HM. The Effect of Robot-Mediated Virtual Reality Gaming on Upper Limb Spasticity Poststroke: A Randomized-Controlled Trial. Games for health journal.
Hu XL, Tong KY, Wei XJ, Rong W, Susanto EA, Ho SK. The effects of post-stroke upper-limb training with an electromyography (EMG)-driven hand robot. J Electromyogr Kinesiol. 2013;23(5):1065–74.
Squeri V, Masia L, Giannoni P, Sandini G, Morasso P. Wrist rehabilitation in chronic stroke patients by means of adaptive, progressive robot-aided therapy. IEEE Trans neural Syst rehabilitation engineering: publication IEEE Eng Med Biology Soc. 2014;22(2):312–25.
Hsieh YW, Lin KC, Wu CY, Lien HY, Chen JL, Chen CC, Chang WH. Predicting clinically significant changes in motor and functional outcomes after robot-assisted stroke rehabilitation. Arch Phys Med Rehabil. 2014;95(2):316–21.
Chen W, Cui X, Zhang J, Wang J. A cable-driven wrist robotic rehabilitator using a novel torque-field controller for human motion training. Rev Sci Instrum. 2015;86(6):065109.
McKenzie A, Dodakian L, See J, Le V, Quinlan EB, Bridgford C, Head D, Han VL, Cramer SC. Validity of Robot-Based assessments of Upper extremity function. Arch Phys Med Rehabil. 2017;98(10):1969–76.
Housley SN, Wu D, Richards K, Belagaje S, Ghovanloo M, Butler AJ. Improving Upper Extremity Function and Quality of Life with a Tongue Driven Exoskeleton: A Pilot Study Quantifying Stroke Rehabilitation. Stroke Res Treat 2017, 2017.
Palermo E, Hayes DR, Russo EF, Calabro RS, Pacilli A, Filoni S. Translational effects of robot-mediated therapy in subacute stroke patients: an experimental evaluation of upper limb motor recovery. Peerj 2018, 6.
Picelli A, Munari D, Modenese A, Filippetti M, Saggioro G, Gandolfi M, Corain M, Smania N. Robot-assisted arm training for treating adult patients with distal radius fracture: a proof-of-concept pilot study. Eur J Phys Rehabil Med. 2020;56(4):444–50.
Bouteraa Y, Ben Abdallah I, Elmogy A. Design and control of an exoskeleton robot with EMG-driven electrical stimulation for upper limb rehabilitation. Industrial Robot-the International Journal of Robotics Research and Application. 2020;47(4):489–501.
Shi XQ, Heung HL, Tang ZQ, Li Z, Tong KY. Effects of a Soft Robotic Hand for Hand Rehabilitation in Chronic Stroke Survivors. J stroke Cerebrovasc diseases: official J Natl Stroke Association. 2021;30(7):105812.
Hwang CH, Seong JW, Son DS. Individual finger synchronized robot-assisted hand rehabilitation in subacute to chronic stroke: a prospective randomized clinical trial of efficacy. Clin Rehabil. 2012;26(8):696–704.
Bishop L, Gordon AM, Kim H. Hand Robotic Therapy in Children with Hemiparesis: a pilot study. Am J Phys Med Rehabil. 2017;96(1):1–7.
Villafañe JH, Taveggia G, Galeri S, Bissolotti L, Mullè C, Imperio G, Valdes K, Borboni A, Negrini S. Efficacy of short-term Robot-Assisted Rehabilitation in patients with Hand Paralysis after Stroke: a Randomized Clinical Trial. Hand (New York NY). 2018;13(1):95–102.
Kuo FL, Lee HC, Hsiao HY, Lin JC. Robotic-assisted hand therapy for improvement of hand function in children with cerebral palsy: a case series study. Eur J Phys Rehabil Med. 2020;56(2):237–42.
Klamroth-Marganska V, Blanco J, Campen K, Curt A, Dietz V, Ettlin T, Felder M, Fellinghauer B, Guidali M, Kollmar A, et al. Three-dimensional, task-specific robot therapy of the arm after stroke: a multicentre, parallel-group randomised trial. Lancet Neurol. 2014;13(2):159–66.
Vanmulken D, Spooren AIF, Bongers HMH, Seelen HAM. Robot-assisted task-oriented upper extremity skill training in cervical spinal cord injury: a feasibility study. Spinal Cord. 2015;53(7):547–51.
Kim GJ, Hinojosa J, Rao AK, Batavia M, O’Dell MW. Randomized Trial on the Effects of Attentional Focus on Motor Training of the Upper Extremity Using Robotics With Individuals After Chronic Stroke. Arch Phys Med Rehabil 2017, 98(10):1924–31.
Chen ZJ, Gu MH, He C, Xiong CH, Xu J, Huang XL. Robot-Assisted Arm Training in Stroke Individuals With Unilateral Spatial Neglect: A Pilot Study. Front Neurol 2021, 12.
Lee KS, Park JH, Beom J, Park HS. Design and Evaluation of Passive Shoulder Joint Tracking Module for Upper-Limb Rehabilitation Robots. Front Neurorobotics 2018, 12.
Kim MS, Kim SH, Noh SE, Bang HJ, Lee KM. Robotic-assisted Shoulder Rehabilitation Therapy effectively improved Poststroke Hemiplegic Shoulder Pain: a Randomized Controlled Trial. Arch Phys Med Rehabil. 2019;100(6):1015–22.
Sale P, Mazzoleni S, Lombardi V, Galafate D, Massimiani MP, Posteraro F, Damiani C, Franceschini M. Recovery of hand function with robot-assisted therapy in acute stroke patients: a randomized-controlled trial. Int J rehabilitation Res Int Z fur Rehabilitationsforschung Revue Int de recherches de readaptation. 2014;37(3):236–42.
Biggar S, Yao W. Design and evaluation of a Soft and Wearable Robotic Glove for Hand Rehabilitation. IEEE Trans neural Syst rehabilitation engineering: publication IEEE Eng Med Biology Soc. 2016;24(10):1071–80.
Orihuela-Espina F, Roldán GF, Sánchez-Villavicencio I, Palafox L, Leder R, Sucar LE, Hernández-Franco J. Robot training for hand motor recovery in subacute stroke patients: a randomized controlled trial. J hand therapy: official J Am Soc Hand Therapists. 2016;29(1):51–7. quiz 57.
Vanoglio F, Bernocchi P, Mule C, Garofali F, Mora C, Taveggia G, Scalvini S, Luisa A. Feasibility and efficacy of a robotic device for hand rehabilitation in hemiplegic stroke patients: a randomized pilot controlled study. Clin Rehabil. 2017;31(3):351–60.
Nam C, Rong W, Li W, Xie Y, Hu X, Zheng Y. The Effects of Upper-Limb Training assisted with an Electromyography-Driven Neuromuscular Electrical Stimulation Robotic Hand on Chronic Stroke. Front Neurol. 2017;8:679.
Aprile I, Germanotta M, Cruciani A, Pecchioli C, Loreti S, Papadopoulou D, Montesano A, Galeri S, Diverio M, Falsini C, et al. Poststroke shoulder pain in subacute patients and its correlation with upper limb recovery after robotic or conventional treatment: a secondary analysis of a multicenter randomized controlled trial. Int J stroke: official J Int Stroke Soc. 2021;16(4):396–405.
Shin JH, Bog Park S, Ho Jang S. Effects of game-based virtual reality on health-related quality of life in chronic stroke patients: a randomized, controlled study. Comput Biol Med. 2015;63:92–8.
Pulman J, Buckley E. Assessing the efficacy of different upper limb hemiparesis interventions on improving health-related quality of life in stroke patients: a systematic review. Top Stroke Rehabil. 2013;20(2):171–88.
Fernández-Vázquez D, Cano-de-la-Cuerda R, Navarro-López V. Haptic Glove Systems in Combination with Semi-Immersive Virtual Reality for Upper Extremity Motor Rehabilitation after Stroke: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health 2022, 19(16).
Wonsick M, Padir TJAS. A systematic review of virtual reality interfaces for controlling and interacting with robots. 2020, 10(24):9051.
Guillén-Climent S, Garzo A, Muñoz-Alcaraz MN, Casado-Adam P, Arcas-Ruiz-Ruano J, Mejías-Ruiz M. Mayordomo-Riera FJJJon, rehabilitation: A usability study in patients with stroke using MERLIN, a robotic system based on serious games for upper limb rehabilitation in the home setting. 2021, 18(1):1–16.
Zanatta F, Giardini A, Pierobon A, D’Addario M, Steca P. A systematic review on the usability of robotic and virtual reality devices in neuromotor rehabilitation: patients’ and healthcare professionals’ perspective. BMC Health Serv Res. 2022;22(1):523.
Babaiasl M, Mahdioun SH, Jaryani P, Yazdani MJD, Technology RA. A review of technological and clinical aspects of robot-aided rehabilitation of upper-extremity after stroke. 2016, 11(4):263–80.
Bessler J, Prange-Lasonder GB, Schulte RV, Schaake L, Prinsen EC, Buurke JH. Occurrence and type of adverse events during the Use of Stationary Gait Robots-A systematic literature review. Front Rob AI. 2020;7:557606.
Housman SJ, Scott KM, Reinkensmeyer DJ. A randomized controlled trial of gravity-supported, computer-enhanced arm exercise for individuals with severe hemiparesis. Neurorehabilit Neural Repair. 2009;23(5):505–14.
Milot MH, Spencer SJ, Chan V, Allington JP, Klein J, Chou C, Bobrow JE, Cramer SC, Reinkensmeyer DJ. A crossover pilot study evaluating the functional outcomes of two different types of robotic movement training in chronic stroke survivors using the arm exoskeleton BONES. J Neuroeng Rehabil. 2013;10:112.
Page SJ, Hill V, White S. Portable upper extremity robotics is as efficacious as upper extremity rehabilitative therapy: a randomized controlled pilot trial. Clin Rehabil. 2013;27(6):494–503.
Cimolin V, Germiniasi C, Galli M, Condoluci C, Beretta E, Piccinini LJJoD, Disabilities P. Robot-Assisted upper limb training for hemiplegic children with cerebral palsy. 2019, 31(1):89–101.
Krebs HI, Saitoh E, Hogan N. Robotic therapy and the Paradox of the diminishing number of degrees of Freedom. Phys Med Rehabil Clin N Am. 2015;26(4):691–702.
Bessler J, Prange-Lasonder GB, Schaake L, Saenz JF, Bidard C, Fassi I, Valori M, Lassen AB, Buurke JH. Safety Assessment of Rehabilitation Robots: a review identifying Safety Skills and current knowledge gaps. Front Rob AI. 2021;8:602878.
Abu-Dakka FJ, Valera A, Escalera JA, Abderrahim M, Page A, Mata V. Passive Exercise Adaptation for Ankle Rehabilitation Based on Learning Control Framework. Sens (Basel) 2020, 20(21).
Martí Carrillo F, Butchart J, Knight S, Scheinberg A, Wise L, Sterling L. McCarthy CJAToH-RI: Adapting a general-purpose social robot for paediatric rehabilitation through in situ design. 2018, 7(1):1–30.
Chisholm KJ, Klumper K, Mullins A, Ahmadi M. A task oriented haptic gait rehabilitation robot. Mechatronics. 2014;24(8):1083–91.
Nielsen J. Usability 101: introduction to usability. Fremont, CA: Nielsen Norman Group. In.; 2012.
Monardo G, Pavese C, Giorgi I, Godi M, Colombo R. Evaluation of patient motivation and satisfaction during technology-assisted Rehabilitation: an Experiential Review. Games for health journal. 2021;10(1):13–27.
Tousignant M, Boissy P, Moffet H, Corriveau H, Cabana F, Marquis F, Simard JJT. e-Health: Patients’ satisfaction of healthcare services and perception with in-home telerehabilitation and physiotherapists’ satisfaction toward technology for post-knee arthroplasty: an embedded study in a randomized trial. 2011, 17(5):376–82.
Andrade RM, Sapienza S, Bonato P. Development of a “transparent operation mode” for a lower-limb exoskeleton designed for children with cerebral palsy. In: 2019 IEEE 16th international conference on rehabilitation robotics (ICORR): 2019: IEEE; 2019: 512–517.
Wang J, Li J, Zhang Y, Wang S. Design of an exoskeleton for index finger rehabilitation. In: 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society: 2009: IEEE; 2009: 5957–5960.
Sampson M, Shau YW, King MJ. Bilateral upper limb trainer with virtual reality for post-stroke rehabilitation: case series report. Disabil rehabilitation Assist Technol. 2012;7(1):55–62.
Zhang K, Chen X, Liu F, Tang H, Wang J, Wen W. System Framework of Robotics in Upper Limb Rehabilitation on Poststroke Motor Recovery. Behavioural neurology 2018, 2018:6737056.
He Y, Eguren D, Luu TP, Contreras-Vidal JL. Risk management and regulations for lower limb medical exoskeletons: a review. Med devices (Auckland NZ). 2017;10:89–107.
Akiyama Y, Yamada Y, Ito K, Oda S, Okamoto S, Hara S. Test method for contact safety assessment of a wearable robot -analysis of load caused by a misalignment of the knee joint. In: 2012 IEEE RO-MAN: The 21st IEEE International Symposium on Robot and Human Interactive Communication: 9–13 Sept. 2012 2012; 2012: 539–544.
Melia M, Geissler B, König J, Ottersbach HJ, Umbreit M, Letzel S, Muttray A. Pressure pain thresholds: subject factors and the meaning of peak pressures. Eur J Pain. 2019;23(1):167–82.
Ferreira F, Chaves MEA, Oliveira VC, Van Petten A, Vimieiro CBS. Effectiveness of robot therapy on body function and structure in people with limited upper limb function: a systematic review and meta-analysis. PLoS ONE. 2018;13(7):e0200330.
Lohse KR, Lang CE, Boyd LA. Is more better? Using metadata to explore dose-response relationships in stroke rehabilitation. Stroke. 2014;45(7):2053–8.
Hayward KS, Brauer SG. Dose of arm activity training during acute and subacute rehabilitation post stroke: a systematic review of the literature. Clin Rehabil. 2015;29(12):1234–43.
Kwakkel, GJp. Intensity of practice after stroke: More is better. 2009, 7:24.
Wilson RD, Chae J. Hemiplegic Shoulder Pain. Phys Med Rehabil Clin North Am. 2015;26(4):641–55.
Tran DA, Pajaro-Blazquez M, Daneault JF, Gallegos JG, Pons J, Fregni F, Bonato P, Zafonte R. Combining Dopaminergic Facilitation with Robot-Assisted Upper Limb Therapy in Stroke Survivors: a focused review. Am J Phys Med Rehabil. 2016;95(6):459–74.
Kafri M, Myslinski MJ, Gade VK, Deutsch JE. Energy expenditure and exercise intensity of interactive video gaming in individuals poststroke. Neurorehabil Neural Repair. 2014;28(1):56–65.
Cuesta-Gómez A, Sánchez-Herrera-Baeza P, Oña-Simbaña ED, Martínez-Medina A, Ortiz-Comino C, Balaguer-Bernaldo-de-Quirós C, Jardón-Huete A. Cano-de-la-Cuerda RJJon, rehabilitation: Effects of virtual reality associated with serious games for upper limb rehabilitation in patients with multiple sclerosis: Randomized controlled trial. 2020, 17(1):1–10.
Laut J, Porfiri M, Raghavan P. The Present and Future of Robotic Technology in Rehabilitation. Curr Phys Med Rehabilitation Rep. 2016;4(4):312–9.
Francisco GE, Yozbatiran N, Berliner J, OʼMalley MK, Pehlivan AU, Kadivar Z, Fitle K, Boake C. Robot-Assisted training of arm and Hand Movement shows functional improvements for incomplete cervical spinal cord Injury. Am J Phys Med Rehabil. 2017;96(10 Suppl 1):171–s177.
Tousignant M, Boissy P, Moffet H, Corriveau H, Cabana F, Marquis F, Simard J. Patients’ satisfaction of healthcare services and perception with in-home telerehabilitation and physiotherapists’ satisfaction toward technology for post-knee arthroplasty: an embedded study in a randomized trial. Telemedicine J e-health: official J Am Telemedicine Association. 2011;17(5):376–82.
Shirley ED, Sanders JO. Patient satisfaction: implications and predictors of success. J bone joint Surg Am volume. 2013;95(10):e69.
Monardo G, Pavese C, Giorgi I, Godi M, Colombo RJGfhj. Evaluation of patient motivation and satisfaction during technology-assisted rehabilitation: an experiential review. 2021, 10(1):13–27.
Kwon SH, Lee BS, Lee HJ, Kim EJ, Lee JA, Yang SP, Kim TY, Pak HR, Kim HK, Kim HYJAoRM. Energy efficiency and patient satisfaction of gait with knee-ankle-foot orthosis and robot (ReWalk)-assisted gait in patients with spinal cord injury. 2020, 44(2):131–41.
Kim DJ, Hazlett-Knudsen R, Culver-Godfrey H, Rucks G, Cunningham T, Portee D, Bricout J, Wang Z, Behal A. How autonomy impacts performance and satisfaction: results from a study with spinal cord injured subjects using an Assistive Robot. IEEE Trans Syst Man Cybernetics - Part A: Syst Hum. 2012;42(1):2–14.
Ramos Muñoz EJ, Swanson VA, Johnson C, Anderson RK, Rabinowitz AR, Zondervan DK, Collier GH, Reinkensmeyer DJ. Using large-scale Sensor Data to test factors predictive of perseverance in Home Movement Rehabilitation: optimal challenge and steady Engagement. Front Neurol. 2022;13:896298.
Akbari A, Haghverd F, Behbahani S. Robotic home-based Rehabilitation Systems Design: from a literature review to a conceptual Framework for Community-Based remote therapy during COVID-19 pandemic. Front Rob AI. 2021;8:612331.
Kutner NG, Zhang R, Butler AJ, Wolf SL, Alberts JL. Quality-of-life change Associated with robotic-assisted therapy to Improve Hand Motor function in patients with Subacute Stroke: a Randomized Clinical Trial. Phys Ther. 2010;90(4):493–504.
Mohammed SA, Shebl AM. Quality of life among egyptian patients with Upper and Lower Limb Amputation: sex differences. Adv Med. 2014;2014:674323.
Rasouli S, Gupta G, Nilsen E, Dautenhahn K. Potential applications of Social Robots in Robot-Assisted interventions for social anxiety. Int J Social Robot. 2022;14(5):1–32.
Kawatsuma S, Mimura R, Asama H. Unitization for portability of emergency response surveillance robot system: experiences and lessons learned from the deployment of the JAEA-3 emergency response robot at the Fukushima Daiichi Nuclear Power plants. ROBOMECH J. 2017;4(1):6.
Treviño LR, Roberge P, Auer ME, Morales A, Torres-Reveron A. Predictors of functional outcome in a cohort of hispanic patients using Exoskeleton Rehabilitation for Cerebrovascular Accidents and Traumatic Brain Injury. Front Neurorobotics. 2021;15:682156.
Acknowledgements
The authors thank the Central Library and Documentation Center of Kerman University of Medical Sciences for providing access to the knowledge base references required for this study.
Funding
This study was supported by the Medical Informatics Research Center of Kerman University of Medical Sciences (Code: 400000856). The funder had no roles in study design, data gathering and analysis.
Author information
Authors and Affiliations
Contributions
Authors’ contributions: KHM and ASH have designed the study, finalized the search strategy and implemented the thematic analysis, AH and KB have searched and screened the articles and extracted the initial codes for data charting. ASH has supervised the whole review process, KHM has contributed in revising the finalizing data analysis and KB and ASH have technically edited and finalized the article. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The protocol of this study was approved by the ethical committee of Kerman University of Medical Sciences) IR.KMU.REC.1400.606).
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Moulaei, K., Bahaadinbeigy, K., Haghdoostd, A.A. et al. Overview of the role of robots in upper limb disabilities rehabilitation: a scoping review. Arch Public Health 81, 84 (2023). https://doi.org/10.1186/s13690-023-01100-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-023-01100-8